Industry
AI can change the game of breast imaging

AI is going to be an indispensable aid in advancing many aspects of radiology. By combining the ability of AI with the ability of human radiologists, one can bring their ability to diagnose the disease to the next level.
The rising global incidence rates of breast cancer, coupled with the severe backlog of women requiring breast cancer screening appointments due to Covid-19, has reinforced the importance of women’s health and early detection of cancer. According to the World Health Organization (WHO), breast cancer has surpassed lung cancer as the most diagnosed cancer globally, with an estimated 2.3 million new cases, and equating to 11.7 percent of all new cancers globally in 2020. Breast cancer also was responsible for just under 685,000 deaths globally in 2020.
As a result of the countable rise of breast cancer incidence globally, there is heightened pressure for government screening programs. However, screening programs alone are not sufficient to help tackle breast cancer mortality rates. It is essential that the accuracy of breast cancer detection is improved, while false positives and missed lesions are also reduced. These factors are forecast to be at the forefront of advancement in breast imaging for both screening and diagnosis.
The market is witnessing a rising trend toward the use of high-resolution 3D imaging, which provides high-quality images, making it easier for the radiologist to detect fine calcifications.
In addition, the introduction of new products in the market is expected to boost the adoption rate among end-users. The earlier generations of mammography systems provided 2D images of the breast, which limits the interpretation quality. 2D mammography systems provide craniocaudal (CC) and mediolateral-oblique (MLO) images. The flat nature of these images makes it difficult for physicians to interpret images and identify tumors due to overlapping of tissues and calcification, which masks cancerous lesions. With the introduction of new 3D-based technology called digital breast tomosynthesis (DBT), it is possible to obtain a 3D image of the breast. This allows radiologists to scan the breast slice by slice and identify abnormalities, which would be obscured in 2D images.
Other global drivers of the breast-imaging market include strengthened awareness on the benefits of breast cancer screening programs, and the need to improve the accuracy of breast cancer detection. This, alongside a patient-centric approach to screening and technological advancements to enhances patient comfort, is an improvement being implemented to increase participation in screening programs, which in turn has driven the uptake of mammography equipment.
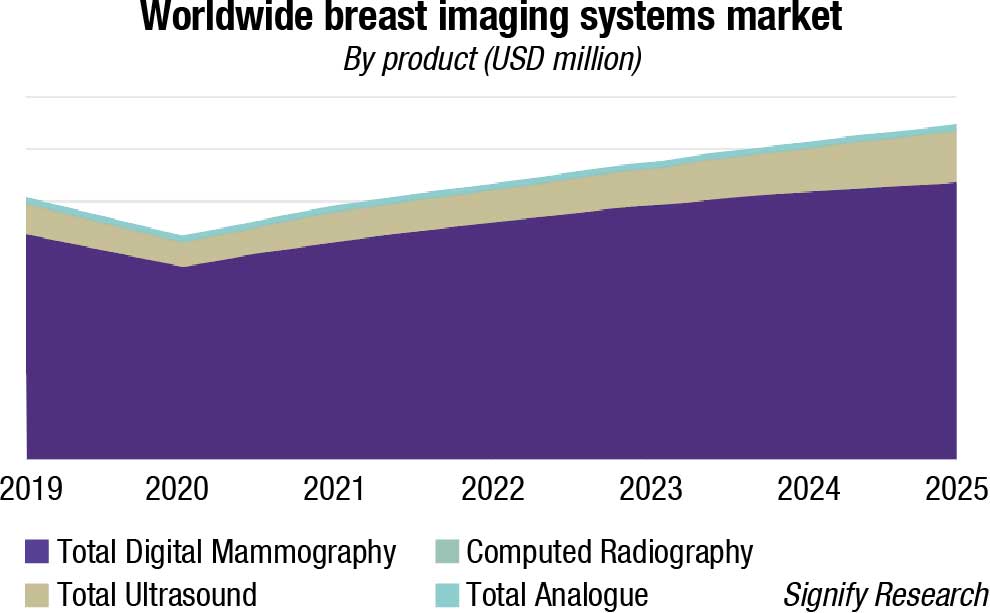
The world market for breast-imaging equipment is forecast to reach almost USD 1.3 billion by 2024, and the breast-imaging artificial intelligence (AI) market is forecast to reach USD 205 million, according to a new report from Signify Research. However, the mammography and breast-ultrasound market revenues declined by just under 15 percent and 18 percent respectively in 2020.
In terms of volume, the global mammography systems market was 6947 units in 2021 and is anticipated to reach 12,688 units by 2027, growing at a CAGR of 10.5 percent.
Breast tomosynthesis system segment in the mammography systems market will showcase growth of 9.4 percent till 2027, led by the growing use of technology in mammography and improved clinical outcomes. The technology provides higher diagnostic accuracy and enhanced efficacy compared to other breast-imaging technologies. Such factors are estimated to foster the segment growth in the coming years. Continuous improvements in clinical outcomes and high-quality visualization of breast tissues are the factors propelling the breast tomosynthesis systems demand.
The device has the capacity to detect cancer at an early stage while reducing the incidence of advanced cancer. The main advantage of the device is that it can reduce the masking effects of surrounding fibro-glandular tissue, thereby improving visualization of normal tissue and breast lesions.
3D mammography technology accounted for USD 475 million in 2021 due to continuous technological advancements in the field of 3D mammography. Thus, the increasing adoption of innovative breast-imaging tools and rising acceptance of DBT devices are contributing to market growth. The introduction of AI in 3D mammography has reduced mammography exam time without compromising image quality. Furthermore, speedy FDA approval for AI-enabled 3D mammography systems is also spurring the market size.
The increasing incidence of cancer cases and rising awareness about early diagnosis of breast cancer are the factors contributing to the market growth. According to the US Breast Cancer Statistics, in 2022, approximately more than 2.8 million new cases of breast cancer are expected to be diagnosed in the US.
Moreover, rising awareness about mortality associated with breast cancer and importance of early screening will further augment the market expansion. Major factors contributing to the growth of breast cancer cases are obesity, reduced childbearing, hormone replacement therapy, and age-related risk factors. The other factors increasing the breast cancer cases are heredity, radiation exposure, having a first child at an older age, and excessive consumption of alcohol.
Thus, with the growing number of people with an inclination toward adoption of such lifestyles, the risk of breast cancer is growing consequently, thereby creating the demand for breast cancer imaging tools in future.
The rising number of product introductions, coupled with increasing FDA approvals, are the factors contributing to the market revenue. The FDA announced new steps in advancing breast cancer screening, and helping patients in acquiring more information pertaining to breast healthcare. These changes include advancement in tissue density standards and adding a new assessment category. Technological collaboration and availability of breast-imaging products are also fueling the market value.
North America dominated the market and accounted for the largest revenue share of 38 percent in 2021. The region is expected to exhibit a considerable growth rate in coming years.
The rising incidence of breast cancer is one of the major factors driving the market in the region. In addition, the presence of highly developed healthcare infrastructure and increasing healthcare spending are among factors anticipated to drive the market in the region over the forecast period.
In Asia-Pacific, the market is anticipated to witness the fastest growth over the next five years. The presence of developing countries, such as China, and Japan, is anticipated to boost market growth in the Asia-Pacific region. In addition, key players are making constant efforts to enter the emerging markets of Asia-Pacific, which is expected to boost the market in coming years.
Some of the major companies operating in the market are Hologic, Analogic Corporation, Canon Medical System Corporation, Fujifilm Holdings Corporation, GE healthcare, and others. These leaders are continuously innovating their products and introducing new products in the market. Rising mergers and acquisitions and licensing and partnership strategies among these players are also augmenting industry expansion.
Some of the key trends in breast imaging include:
Use of 2D versus 3D mammography in screening programs. The United States is the only country that currently uses 3D mammography for screening, with all other countries only using this technology for diagnostic purposes. Western-European countries are expected to be the next to adopt 3D mammography screening programs, but this is not anticipated to happen until the next two to three years.
Changes in demographics of women being screened. Healthcare providers are considering changing breast cancer-screening policies to include younger demographics to help reduce breast cancer-related deaths, and increase early detection. However, the possibility of over-diagnosis and false-positives is still prevalent.
Personalized risk-based screening. The extensive number of factors, which could contribute to the risk of breast cancer, include genetics, family history, polygenic risk scores, and high mammographic density. Personalized risk-based screening may also identify high-risk women for more intensive screening, such as magnetic resonance imaging (MRI) follow-up after mammography. Alternatively, low-risk women may be more suited to longer intervals between screening, which also reduces the risk of false-positives through over-screening.
Use of multi-modality imaging for breast cancer screening. Movement toward risk-based screening is likely to encourage the use of multi-modality imaging. As women are segregated into groups, identified factors, such as increased breast density, are expected to facilitate supplemental screening that are not commonly practiced today.
Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the X-ray film is replaced by electronics that convert X-rays into mammographic pictures of the breast. These systems are similar to those found in digital cameras, and their efficiency enables better pictures with a lower radiation dose. These images of the breast are transferred to a computer for review by the radiologist and for long-term storage. The patient’s experience during a digital mammogram is similar to having a conventional film mammogram.
There continues to be a significant discrepancy across the world with regards to screening programs. Countries with large populations, like China and India, for example, do not have a formal, structured approach to screening. There are also large differences in participation even in regions where formal programs exist, such as in Western Europe.
In Spain, Denmark, and Finland there is around 80-percent participation, whereas participation rates in other countries like France, the DACH region, and Portugal are all significantly below the 50-percent mark. The European Union is attempting to increase participation and move the adoption rates to 80 percent or above.
Predict risk of breast cancer using AI. The automated technique of breast cancer detection that is still being considered is screening X-ray mammography by radiologists, which sometimes leads to false-positive and false-negative results, in turn increasing the mortality ratio in breast cancer patients. However, an earlier study shows that AI can be used as a detecting aid for radiologists where either radiologists or AI can work hand in hand, or AI can be used as the second opinion for better results.
Predicting future health outcomes for patients at an individual level will allow physicians to deliver care more quickly to those who need it most, while preventing future harms and improving outcomes. AI is transforming the medical device space with its powerful ability to learn and predict trends and patterns. In a new study published in the journal Radiology, Dr Dembrower and colleagues trained a sophisticated type of AI, called a deep neural network, to predict which women are at future risk of breast cancer.
Screening for breast cancer is recommended for women over the age of 45, and every two years after the age of 55. Yet, this one-size-fits-all approach is not optimized for cancer detection for women who are at a higher risk. Risk prediction is a crucial building block toward developing individually adapted screening. Mammogram images that are rich with information, such as breast density, high breast density, or a greater amount of glandular and connective tissue compared to fat, are considered a risk factor for breast cancer. Leveraging all of the information contained within an image is a complex task and one that has been the focus of many research groups.
This study takes full advantage of all the rich information found in mammograms, which has the potential to identify women at higher risk and who would benefit from additional screening, such as with MRI. In the study, the deep neural network was developed and trained on over two million mammograms – an unprecedented size for an image data set. This deep neural network showed a higher risk association for breast cancer compared to the current best mammographic density model, and did not display the same bias as the density-based model.
Currently, mammographic density is not reported, and the introduction of an individually adapted screening, using a deep neural network, such as the one developed by Dr Dembrower and colleagues, has the potential to predict cancer.
AI is going to be an indispensable aid in advancing many aspects of radiology. By combining the ability of the AI with the ability of human radiologists, one can bring their ability to diagnose the disease to the next level.
Breast cancer – The best protection is early detection!
 Suresh Sharma
Suresh Sharma
Chairman-cum-Managing Director,
Allengers Group of Companies
Amongst the most dreaded of all life-threatening diseases is cancer, a silent killer. Cancer takes a huge toll on women world-wide. It is difficult to imagine anyone who has not heard of this dreaded disease. Cancer is a renegade system of growth that originates within a patient’s biosystem, more commonly known as the human body. Breast cancer is one of the most prominent ones.
Though major advances are taking place in the diagnosis and treatment of cancer, yet the challenges to contain it are growing by the day. However, because of early detection, intervention, and postoperative treatment, breast cancer mortality has been decreasing.
Why mammography? Women worldwide have one-in-seven risk of developing breast cancer. The risk of breast cancer increases with age. So it is all the more important for women above 40 years of age to have screening mammogram annually. Approximately 1.2 million breast cancer cases are diagnosed globally every year with about 75 percent of them in women over the age of 50. About 12 perent of all women will get breast cancer in a lifetime.
Benefits of mammography. A mammogram can detect up to 90 percent of breast cancers and is the only proven means of detecting breast cancer. Screening mammograms may detect a very small cancer, much before the patient or the doctor can actually feel it. Breast cancer cannot be prevented, but earlier a breast cancer is detected, better is the chance of its successful treatment. The goal of mammography is the early detection of breast cancer, typically through detection of characteristics like calcifications, masses, asymmetries, and distortions.
The technology. Mammograms can often show abnormal areas in the breast. They cannot depict for sure if an abnormal area is cancer, but they can help the specialist decide if further investigation (such as a breast biopsy) is needed.
Along with the inclusion of breast-density measurement software, AI-based CAD, CEDM, etc., currently 3D mammography with tomosynthesis is becoming the basic need for breast imaging. This technique has helped a lot in case of dense-breast imaging and with time to come this technique will be used more for effective breast diagnosis.
You can’t fight if you don’t know. On an average, getting a mammogram should take only 15 minutes – but these 15 minutes could save one’s life!
Mammograms will continue to play a fundamental role in the detection of breast cancers, but the occurrence of false-positives often leads to benign lesions being operated on. With heightened pressures for breast cancer screening programs to account for the rising female population qualifying for mammography screening, it is crucial that the number of false-positives subsequently does not rise as a result. Advanced techniques in mammography screening, such as AI, tomosynthesis guided biopsy, contrast-enhanced spectral mammography, as well as a more personalised approach to breast cancer screening are initiatives that could help reduce the number of false-negatives or positives and drive more accurate early detection of breast cancer.
AI is still in the stage of weak AI. Although it has made rapid developments in the medical field in the past decade, it is far from the goal of being fully integrated into the work of clinicians and large-scale application in the world. At present, there are many limitations in CAD systems for breast cancer screening, such as the lack of large-scale public datasets, the dependence on ROI annotation, high image-quality requirements, regional differences, and overfitting and binary classification problems.
In addition, AI mostly aims for one-task training and cannot solve multiple tasks at the same time, which are the challenges and difficulties that DL faces in the development of breast imaging.
Meanwhile, these also provide a new impetus for the development of breast-imaging diagnostic disciplines and show the broad prospect of intelligent medical imaging in the future.
In addition to their application in traditional imaging methods, CAD systems based on DL are developing rapidly in the fields of digital breast tomosynthesis, ultrasound elastography, contrast-enhanced mammography, ultrasound, and MRI. Experts believe that AI in breast imaging can not only be used for the detection, classification, and prediction of breast diseases, but also further classify specific breast diseases (e.g., breast fibroplasia) and predict lymph node metastasis and disease recurrence. With the progress of AI technology, radiologists will achieve higher accuracy with higher efficiency and more accurate classification and determination of adjuvant treatment for breast diseases to achieve early detection, early diagnosis and early treatment of breast cancer, and benefit the majority of patients.












