Anesthesia Equipment
Anesthesia industry this year and beyond
While there is no telling exactly what medical breakthroughs will occur in the coming months and years, some of the developments anesthesia market has encountered recently are excellent indicators about where the industry is headed this year and beyond.
Today’s ever-changing healthcare environment presents unique challenges for hospital administrators and executives, policy-makers, and healthcare providers alike, especially when it comes to ensuring patient access to safe, high-quality, and cost-effective anesthesia care.
The current healthcare systems are overwhelmed with ever-expanding advances in the treatment modalities to provide safe and cost-effective patient care. For new digital healthcare technologies to reach their full potential, without the need to increase resources, the whole health and care system will need to anticipate and plan for the future. One of the challenges for these integrated digital health systems is supporting perioperative clinical decision-making.
The safety and quality of anesthesiology care has improved at least 10-fold throughout the past 20 years. Unfortunately, anesthesiology still does contribute to major and avoidable complications and deaths, and is still not completely safe for patients. Several top market vendors are working to achieve zero-defects in anesthesiology. Furthermore, newly developed medications, devices, technology, and clinical-decision support tools are making anesthesiology more easy and comfortable for patients.
Major Vendors in Indian Anesthesia Equipment Market – 2019* |
|||
|---|---|---|---|
| Tier I | Tier II | Tier III | Tier IV |
| GE | Drager & Mindray | BPL, Meditec England, Comen, & Spacelabs | Skanray, Allied Medical, Aeon Medical, and local & regional brands |
| *Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian anesthesia equipment market. | |||
| ADI Media Research | |||
Indian market
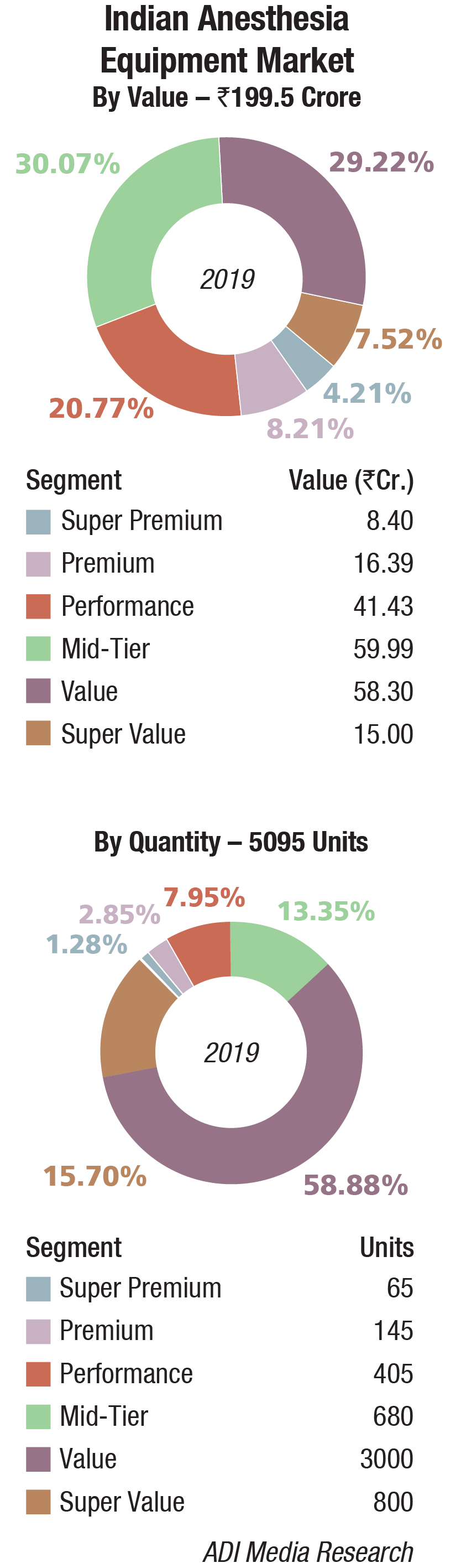
The Indian anesthesia equipment market in 2019 is estimated at Rs 199.5 crore, at 5095 units.
GE is the clear leader. Drager and Mindray are vying for the second slot. BPL, Meditec England, Comen, and Spacelabs are also aggressive in this segment. Skanray, Allied Medical, Rohanika (marketing products from Aeon Medical), and other local and regional brands also have presence.
The NXT 9100c model of GE was popular with the government in 2019. Also, 91 units of model 660 were procured from GE Healthcare by the West Bengal government. HLL procured 56 numbers of NXT from GE and 29 units from Avance. Three million units are expected to be bought by HLL in 2020. ESI is also expected to close its order of 64 units in the coming year, and so is PGI, Chandigarh.
 The mid-priced segment is gradually increasing its share, and is largely catered to by GE, Drager, and Mindray, each trying to cement its share with new product launches and upgradation of value models with software and some other features add-ons.
The mid-priced segment is gradually increasing its share, and is largely catered to by GE, Drager, and Mindray, each trying to cement its share with new product launches and upgradation of value models with software and some other features add-ons.
Global market
The global anesthesia devices market is expected to reach USD 14,783 million by 2024, with an anticipated CAGR of 7.11 percent, predicts Mordon Intelligence. The increasing integration of technological advancements is one of the key factors expected to boost anesthesia devices market growth during 2019 to 2024. Technological advancements help the stakeholders of the healthcare industry to focus on improving the precision and effectiveness of anesthesia delivery, increasing patient safety, and minimizing the wastage of anesthetic gas. New-generation anesthesia devices are further focusing on minimizing the instances of accidental incidents during anesthesia delivery by incorporating safety features. These technologically advanced devices also help clinicians in working closely with their patients while eliminating the need for extra-long breathing circuits, eventually preventing any losses to the system compliance.
The risk of contamination with the use of anesthesia machines during surgical procedures is an important negative for the anesthesia machines. This is mainly because the chances of bacterial infections are getting higher with an increasing number of surgeries and use of anesthesia machines. Many anesthesia machines are often colonized by microorganisms. One such example is an anesthesia machine’s outer region, which contains bacterial species that may be transferred from the machine to the anesthetist and then to the patient, resulting in bacterial contamination and infection.
The use of computer-controlled anesthesia machines is an emerging trend in the anesthesia machines market. Computer-controlled anesthesia machines help in reducing the patient’s pain during surgical procedures, and also provide features such as alarms to notify if in case of an emergency or backup it is required to switch off the defected pipeline or cylinder.
Some of the major players in the market are GE Healthcare, Dragerwerk, Smith Medical, Spacelabs Healthcare, Covidien, Mindray, and Medtronic.
Current trends in anesthesiology
One of the most fascinating things about medicine, and anesthesiology in particular, is the near-constant advances in medical technology and their implications. While there is no telling exactly what medical breakthroughs will occur in the coming months and years, some of the developments market has encountered recently are excellent indicators about where the industry is headed this year and beyond.
Pharmacogenetics testing will become standard clinical workflow to the point that pharmacotherapy will be personalized to an individual patient, based on their predicted response to that therapy. Improvements in medication management, based on a patient’s genotype, will drive down opioid usage and further advance enhanced recovery care pathways.
Non-invasive cardiac output measurement will become just another routine vital sign that incorporates into pre-operative testing, perioperative monitoring, and PACU care. The ability to non-invasively assess advanced hemodynamics continuously at the bedside will take a lot of guesswork out of perioperative management.
Anesthesia information management systems (AIMS) with intraoperative monitoring-device connectivity will provide powerful decision support tools with real-time clinical guidance, utilizing machine learning algorithms to predict things like hypotension long before it occurs clinically.
Artificial intelligence (AI) will transform patient care with advanced early warning systems (EWS) that utilize wireless surveillance to leverage algorithms for pattern recognition, allowing computers to detect slight variations in data with human-applied clinical rules (algorithms) that recognize patient deterioration and automatically activate interventions like rapid response teams, making found dead in bed a never event.
Cardiovascular imaging with AI software will automate calculation of left ventricular ejection fraction, making this a new standard vital sign for procedures, using intraoperative cardiac echography.
Pre-operative testing will be performed in virtual clinics by a cognitive assistant-type platform that will complete repetitive tasks and engage patients through interactive patient portals to capabilities, and a wide range of clinical knowledge, this automated routine work will support clinical decision-making, and free clinicians to focus more on direct patient communication and complex care decisions.
Patients will have 24/7 access to virtual nurse avatars who will help manage home medications and provide health assistance and coaching on healthier choices that support lifestyle changes.
Wearable home devices will be able to detect an asthma attack before it happens and new biosensor devices with ECG electrodes and triple-axis accelerometers will track heart rate, rhythm, breathing, temperature, steps, and even detect body position in case a person has fallen. They will be no longer need to ask patients how active they are or if they have had any falls or have been compliant with pre-habilitation exercises because these devices will be able to share this information to improve shared decision-making with the patients.
Ingestible sensors and drug-device combination products will be able to monitor medication effectiveness and offer the ability to objectively track patient compliance. Imagine better-supporting families, who are caring for family members with dementia or serious mental illness, or even confirming the absence of illegal drugs to improve patient care and outcomes.
A new novel anesthetic agent will be available that combines the sedative-hypnotic drug properties of current medications with a rapidly titratable intravenous delivery system, with a high therapeutic index and minimal side effects. This will go beyond small modifications of current medications like a proposed remimazolam and move us into a new generation of anesthetics yet to be discovered.
The next 10 years will be challenging, no doubt; the redesigning of healthcare delivery will develop to meet the demands of new payment methodologies while pursuing continued innovation that personalizes patient-specific care, improves vigilance and patient safety through machine learning, virtual assistants, and early warning surveillance systems.
Way forward
At some point in the future, if a fully autonomous anesthesia system could be created and validated, then it could certainly result in profound effects on the workflow patterns and needs of anesthesia providers. These innovations may allow anesthesiology the freedom to reinvent itself from an intraoperative specialty to one of true perioperative medicine. Such changes are already underway, with emphasis on non-operating-room subspecialties like pain medicine and critical care. For the time being, though, both the hopeful and dystopian futures are possible, and there is no way to reliably predict which outcome is more likely. As a specialty, anesthesiologists have tended to be early adopters of technology, and tend to be comfortable incorporating technological solutions to improve patient care. They should continue this trend and not only stay abreast of advances in AI, but also make concerted efforts to integrate them into practice now, so that they can be the authors of their own future, improving provider productivity and each patient’s outcome by building and working in concert with narrow AI learning systems that create truly individualized, evidence-based clinical guidelines built in real time, based on analysis of the entirety of medical literature and pooled patient data from electronic medical records.
Industry Speak
 Manju Goyal
Manju Goyal
National Sales Manager – Life Support,
Mindray Medical India Pvt. Ltd.
Electronic gas mixer – An intelligent and reliable partner
Over many years in anesthesia, we have seen transition from Boyles apparatus to external ventilator machines to integrated ventilators, (two gas version). Now, we have come very far with three gas machines having various ventilation modes. We have often experienced the conversation between cascaded flow meters and electronic flow meters, which one is more user friendly, accurate, safe, and so on. But as both of these technologies have mechanical way of mixing, so the only way you see the fresh gas flow (as flow tubes or digital) changes, but for machine internally its mechanical mixing only. So, both have the same kind of limitations like setting independent flow for each gas, and the user spends a lot of attention in titration of adequate flows to meet minimal flow anesthesia and maintain the balance of anesthesia. As the case progresses, we need to manually adjust O2 as per change in the patient’s uptake.
All this extra work can be managed if you have an intelligent and careful technical partner. That can be your anesthesia machine with electronic gas mixer. This will take titration job of gases on itself and will take away some concerns including leaks. Many anesthetists have a concern – what flows are adequate for delivering set tidal volume at the lowest fresh-gas flow. In this regard, they again do a titration work to set adequate flow and in case leak starts that flow needs to be changed again. This extra load you can leave on your intelligent anesthesia machine to do. The mixer will inform you that your gases are not enough for tidal volume delivery, or if these are more than what actually you need. This will be more reliable as feedback comes from heart of the machine not from external signs.
Electronic gas mixing is a well-established technology in ICU ventilators, and it has been found very reliable over the years in anesthesia machines as well. This demand has set to increase as anesthetists can very well benefit from this technology, and the cost of operation can also be reduced.
Industry Speak
 Pradeesh CB
Pradeesh CB
National Product Manager-Critical Care and Anesthesia,
BPL Medical Technologies Pvt. Ltd.
Anesthesia market trends
Anesthesia machines are used inside operating rooms to facilitate administration of anesthesia to patients who undergo a surgical procedure. Anesthesia machines do many functions such as supply compressed gases, measure flow of gases, add vapors in known concentrations, deliver the gas mixture to patient via a breathing system, mechanical ventilation, scavenge waste, and monitor patient parameters with safety alarms.
It is evident that the market is moving toward a fully integrated system. Most of the hospitals are upgrading their old basic anesthesia delivery system to anesthesia workstations with comprehensive patient monitoring system. Modern anesthesia machines use advanced electronics, software, and technology to offer extensive capabilities for ventilation, monitoring, inhaled agent delivery, low-flow anesthesia, closed-loop anesthesia, electronic record keeping, and so on. These developments have really helped the clinicians to deliver safe anesthesia to their patients.
Two-gas or three-gas system, with dual cascaded tubes along with a fully integrated ventilator, which supports control and support ventilation mode, is still the highest selling product. Many vendors are improving this segment by adding better features, such as integrated EtCO2 and gas measurements, dual flow sensing for better ventilation control, electronic flow measurements, bigger screen for accommodating more patient parameters, and low and minimal flow application.
More and more users are showing interest in electronic flow control, which is with better accuracy, especially for low- and minimal-flow anesthesia applications. With electronic flow control, the consumption also can be monitored. This help in saving gases and costly agents. Integrated anesthesia gas module, combined with patient monitor having depth of anesthesia and muscle relaxation monitoring, brain function monitoring, and the like, are commonly seen on such high-end anesthesia workstations.
Digital fresh-gas control with closed loop system along with electronic delivery of anesthetic agents will be the future. Connectivity solutions are available with many players so that hospital can have paperless OR. Currently, this type of solution is available at a premium price point.
MRI-compatible anesthesia machine is becoming more popular and is sometimes also treated as a statutory requirement inside the MRI room. Nowadays, most of the new purchase of MRI equipment is packaged with MRI-compatible anesthesia machine, MRI compatible patient monitor, MRI compatible pumps, laryngoscopes, suction, and the like.
For small setups, portable anesthesia machines are also available in the market. The advantages of the portable machine are: it occupies less space, it is light weight and so easy to transport, and it can be easily mounted on rails. The table-top version, lower in price, is also available.
Second Opinion
 Dr Dipankar Dasgupta
Dr Dipankar Dasgupta
Director, Department of Anesthesia,
Jaslok Hospital and Research Centre
Anesthetic depth monitors
It was 16th October 1846 when the world was shaken with the advent of general anesthesia. It has taken over 175 years for this specialty to get modernized. Concretization of this specialty was possible in 1933 with Henry Dale’s discovery of neuromuscular transmission with acetylcholine, along with the therapeutic use of neuromuscular blocker d-tubocurare by Harold Griffith and Johnson. Then, was the march of newer muscle relaxants, along with newer molecules of inhalational anesthetics. The progress was compounded with anesthesia and drug delivery system. Dignity of the specialty has galloped with anesthesia equipment, and the ultimate is the safety equipment. In this current publication, I will stress upon anesthetic depth monitors.
Diethyl ether – chloroform trichloroethylene era – the safety was practiced by Dr Guedel’s four stages and four planes. Subsequently, cerebral-cortex monitoring started with ECG, MAC values, BIS, and entropy. At any given time during anesthesia these clinical data will assert the CNS. These numerical values in association with hemodynamics and respiratory will govern essential physiological parameters. Now, most of the depth of anesthesia monitor (DOA) investigate the ECG as a surrogate parameter of anesthesia depth. The most common monitors bispectral index (BIS) monitor, entropy module, and narcotrend monitor transfer the raw EEG signal into a power spectrum by applying fast Fourier transformation (FFT) to the signal.
EEG is the oldest monitor to measure depth of anesthesia. The raw EEG is obtained using standard 19-electrode method; however, this is time-consuming and impractical, and requires expert interpretation. BIS is a derived value, based on EEG recordings, on a normalized scale of 0 to 100, where appropriate hypnosis is thought to occur in the range of 40–60.
Another example of depth monitor is the narcotrend monitor that uses a different algorithm to analyze the raw EEG-signal patterns. The main depth of anesthesia measures include the narcotrend stage-ranging from stage A (awake) to F (deep to profound anesthesia) – and narcotrend index – ranging from 100 (awake) to 0 (no electrical activity detected), in addition to trend data among many other EEG and EEG-related parameters.
Entropy was introduced by Datex Ohmeda company is 2003. The signals are divided into state entropy (SE) and response entropy (RE). Both are dimensionless numbers between 91 and 0 and 100 and 0 respectively. SE is based on EEG alone but RE is based on EEG and electromyography. The use of brain-monitoring devices can lead to reduction of intraoperative drug consumption, reduced incidence of postoperative drug consumption, reduced incidence of postoperative nausea and vomiting, facilitate recovery from anesthesia compared to routine care, and can also lead to a reduction of intraoperative awareness.
Biomedical engineering is advancing at an Olympic speed and the future lies with not mere CNS, respiratory, cardiovascular, and metabolic need, but the detail physiology at cellular level.
Second Opinion
 Dr Anil Kumar Jain
Dr Anil Kumar Jain
Senior Consultant & Co-Chairperson,
Department of Anesthesiology, Pain and Perioperative Medicine,
Sir Ganga Ram Hospital
The limitless scope of anesthesiology – What’s next in evolution
Anesthesiology is a complex branch of medicine. With enhanced safety and effectiveness of perioperative anesthesia care, more and more patients are coming forward to have surgical interventions. This has a progressive impact on ever-increasing burden on anesthesia healthcare system. Initially, anesthesiologists were much concerned about their clinical skills around hemodynamic physiology, managing children, elderly and pregnant patients, but lately they have shifted their focus onto systems (liver, kidney), neuro cognition (dementia delirium), and myocardial processes. In order to optimize anesthesia care, multipronged strategies have to be adopted, which may entail a combination of advanced monitoring devices, pharmacological intervention, and perioperative management.
Newer anesthesia drugs, inhalation agents, such as, desflurane, sevoflurane, and propofol are fine drugs but still safer anesthetics are desirable to enhance specific organ protection. To this effect, anesthetic drugs, which have profound affect when in use but not traceable in body on conclusion of anesthesia, are needed. Also, agents which could be administered by simple easy-to-use equipment would be highly appreciated.
Conventionally, during anesthesia, cardiac and pulmonary systems can be well managed by invasive monitoring; but we require efficient, intelligent, and accurate noninvasive monitors, especially which could tell us about hemodynamic profile more consistently. Simpler echocardiography probe and monitors, which could self-diagnose problems noninvasively, would help conduct of safe anesthesia.
The kidney-function monitor, which when placed noninvasively over the renal area, should be able to monitor renal perfusion, pressures, and oxygenation. Such a monitor, if made available, will facilitate decreasing acute kidney injury incidences.
The cerebral brain-function monitor and the cerebral doppler are in use but have not helped in decreasing incidences of delirium and cognitive dysfunction. Refined brain-function monitors, encompassing physiology, biochemistry, electroencephalography, and oxygenation may help in maintaining brain’s internal milieu in pre-anesthesia state, to decrease delirium postoperatively.
Hepatobiliary system is neglected by the present anesthesia management. Noninvasive and concurrent monitoring of liver physiology, pharmacology, oxygenation, and vital functions may add to the safety of anesthesia.
Anesthesia has become safe, as far as mortality is concerned, but morbidity-safe anesthesia would be furthered by focusing on renal, hepatic, and cerebral monitoring. Noninvasive and intelligent monitors are the need of the day.











