MB Stories
Automation, automation, and automation
The coagulation testing market share is poised to grow significantly over the next few years, with great strides made in automation providing the requisite impetus.
The pandemic helped put in perspective, importance of healthcare workers. We continue to have shortages of medical laboratory scientists – and supplies. There were crunches during the pandemic such that the easier the device was to use, the more sustainable the whole process. And that is where automation received its momentum – not only for routine tests but also for some of the more esoteric tests that require manual processes. The more automated it is, the better it is for us, so we do not need specialized medical laboratory scientists.
And automation is not just connecting the track systems or the inside of the box, but also about middleware and what the software can do to make running the tests easier. Track systems, integration into larger track systems, and the automation that goes in the box of coagulation analyzers, like HIL (hemolysis, icterus, lipemia) modules are all changing. Coagulation is late to the game in terms of incorporating HIL into the workflow compared with chemistry, which has been doing this for some time.
No doubt, things are getting much better at what is done in the coagulation lab, for instance, the ristocetin cofactor assay, the classic way of measuring the activity of von Willebrand factor [VWF]. This was done on a platelet aggregometer until about 15 years ago. Now there are automated von Willebrand activity assays that can be put on instruments. That is huge for monitoring patients who are on therapy in the hospital. And there continues to be shortage of medical laboratory staff (MLS) to perform the old aggregometry method every day, so putting it on the instrument is a huge win. Another win is the availability of rapid heparin-induced thrombocytopenia testing on automated instruments – getting those results rapidly not only saves money in argatroban costs, it is better patient care.
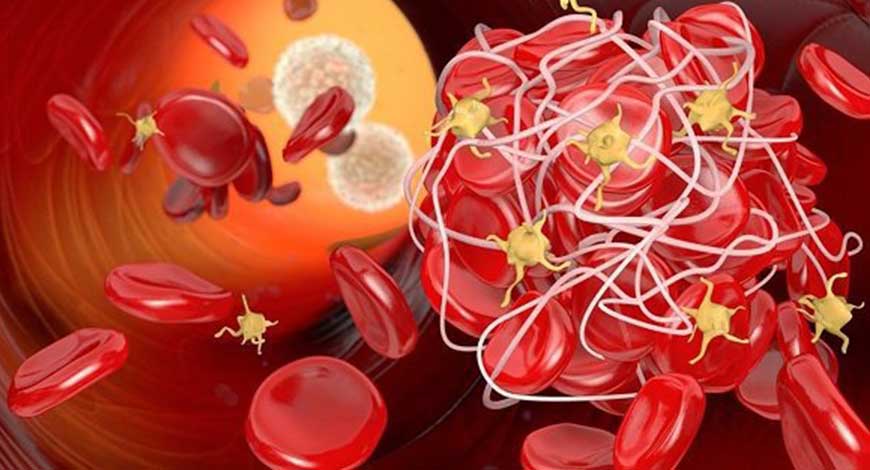
Numerous advantages, including high-volume testing, improved reproducibility, user flexibility, time and cost savings, and increased accuracy with quality controls, resulted from the automation of coagulation procedures. Instruments used in coagulation gradually changed as new technologies were integrated into them. These technologies included chromogenic substrates, latex agglutination immunoassays, turbidimetry, and optical detection of clot formation.
Automation in coagulation testing is not new. But there have been developments seen in coagulation testing. Automated analyzers have become an integral part of testing where manual handling is not required and testing is done on automation.
The coagulation laboratory is a dynamic setting with automated analyzers that provide improvements in test volume and diversity. Innovations in hardware and software enable random access testing with multitest profiles. Prothrombin time (PT) with the international normalized ratio (INR), partial thromboplastin time (PTT; also known as the activated partial thromboplastin time [APTT]), fibrinogen, thrombin time, and D-dimer assays were previously on the menu of standard coagulation tests.
The introduction of new coagulation methodologies has further improved testing capabilities in the coagulation laboratory. Refinement of these methodologies has allowed the use of synthetic substrates and measurements of single proenzymes, enzymes, and monoclonal antibodies, which increases the ability to recognize the causes of disorders of hemostasis and thrombosis.
These include assay end-point detection principle, mechanical end-point detection, photo-optical end-point detection, nephelometric end-point detection, and immunologic light absorbance end-point detection.
With new advancements made in the capability and flexibility of coagulation instrumentation, the industry is seeing a positive change. Today, newer models of instrumentations are fully automated, and have multiple factor analyses across runs that are standardized, easy to use, and quality controlled.
In the past, instruments required manual pipetting, recording, and computing the data, all of which required a significant amount of operator experience, time, and effort. Today’s technology enables a walkaway environment where the operator can carry out other duties after loading the specimens and reagents and starting the testing sequence.
Coagulation analyzers were only able to measure the optical density of a clot in a cuvette. They were operated mechanically, using a hook to detect a clot in the cuvette. However, with the advancement in technology in time, this has now been replaced by simultaneous detection of clotting factors via clotting, colorimetric, and immune principles.
Although clot-detection techniques have remained constant, the emergence of chromogenic- and immunologic-based assays necessitated the addition of new equipment to the coagulation laboratory. To increase the test menu options, many techniques were merged into a single analyzer. Clinical laboratory equipment that could conduct both clot-based and chromogenic-based assays on one platform was created from instruments that could only perform clot-based assays. The creation of a single device that could conduct clotting, chromogenic, and immunologic assays was the next stage. Improvements in specimen and reagent processing, throughput, data management, and result traceability are some more advancements.
In the days of visual methods, coagulation assays were carried out twice in the days of visual methods to lower the coefficient of variance, which typically surpassed 20 percent. Although the precision of semiautomatic devices has increased, repeat testing is still necessary due to the need for manual pipetting of chemicals and plasma. Precision has increased to the point that single testing may be confidently carried out while reducing material and reagent costs with the introduction of fully automated devices. It has been possible to attain coefficients of variation that are less than 5 percent, and in certain cases even less than 1 percent. For all equipment and reagent combinations, initial accuracy and precision are established through in-lab technique validation.
Modern technologies are pushing demand for testing. Some popular ones are:
Improved specimen management. Primary tube sampling. Many coagulometers encourage the operator to place the primary collection tube on the instrument after centrifugation, which eliminates the need to separate the plasma into a secondary tube. In addition, instruments often accommodate multiple tube sizes. Significant time savings occur as a result of elimination of the extra specimen preparation step, and errors resulting from mislabeling of the aliquot tube are reduced.
Closed-tube sampling has improved the safety and efficiency of coagulation testing. After centrifugation, the tube is placed on the analyzer without removing the blue stopper. The cap is pierced by a needle that aspirates plasma without disturbing the red blood cell layer. Not only does closed-tube sampling save staff time, it also reduces the risk of specimen exposure through aerosols or spillage. Closure also promotes plasma pH stabilization. When closed-tube sampling is used, specimens are visually checked for clots after centrifugation by looking for the presence of fibrin strands. For example, if the assay result is a short clotting time (or the corresponding coagulation tracing available on some instruments) is abnormal then the sample will be rimmed with wooden sticks to determine if a clot is present.
Flagging for specimen interferences. Some analyzers monitor the quality of the test specimen for interfering substances or unusual testing characteristics, such as hemolysis, lipemia, bilirubinemia (icterus), abnormal clotting patterns, or results that fall outside the linear range of the reference curve (values above the top point or below the bottom point of the calibration line). Flags warn the operator of potential errors so that problems can be resolved in a timely manner (see later).
Automatic dilutions. Many instruments perform multiple dilutions on patient specimens, calibrators, or controls, eliminating the need for the operator to perform this task manually, and reducing the potential for dilution errors. These conditions can be automatically programmed into the individual test setups on the analyzers being used.
Expanded computer capabilities. The computer circuitry of analyzers now incorporates internal data storage and retrieval systems. Hundreds of results can be stored, retrieved, and compiled into cumulative reports. Multiple calibration curves can be stored and accessed. Quality control files can be stored, which eliminates the time-consuming task of manually logging and graphing quality control values. Westgard rules can be applied, and failures are automatically flagged. Some analyzers feature automatic repeat testing when failures occur on the initial run. The quality control files can be reviewed or printed on a regular basis to meet regulatory requirements.
The programming flexibility of modern analyzers has enhanced the laboratory’s opportunities to provide expanded test menus. Most advanced analyzers are preprogrammed with several routine test protocols ready for use. Specimen and reagent volumes, incubation times, and other testing parameters do not need to be predetermined by the operator but can be changed easily when necessary. Additional tests can be programmed into the analyzer by the user, whenever needed, which allows for enhanced flexibility of the analyzer and reduces the need for laboratories to have multiple instruments.
Instrument interfacing to laboratory information systems and specimen bar coding capabilities have become a priority as facilities of all sizes endeavor to reduce dependence on manual record keeping. Bidirectional interfaces improve efficiency through the ability of the instrument to send specimen bar code information to the laboratory information systems and receive a response, listing the tests that have been ordered. This eliminates the need for the operator to program each specimen and test.
Improved flagging capabilities alert the operator when preset criteria have been exceeded. Flags may indicate instrument malfunction, such as cuvette jams, low reagent volume, and temperature errors, or a problem with the results, such as values that exceed critical limits, inability to detect an accurate end-point, or values outside of the linear range.
Smartphone-based blood coagulation tests. Besides various testing modules present in the market along with the home PT/INR testing modules, there is a new module grabbing the attention of the industry – a proof-of-concept system that uses the vibration motor and camera on existing smartphones to perform PT/INR testing. This smartphone-based coagulation testing is becoming popular among the end users too.
This new technology, still in the proof-of-concept stage will help improve time within the therapeutic range for anti-coagulation users, particularly in rural areas.
Under the automated technology, all reagents are automatically pipetted by the instruments. Specimen may or may not be pipetted. Analyzers contain monitoring devices and internal mechanism to maintain and monitor constant 37° C temperature throughout testing sequencing. Timers and initiated and clot formation is detected automatically.
Improved reagent handling. Automated and semiautomated coagulometers now have the capability to perform tests on smaller sample volumes. Traditionally, PT assays required 0.1 mL of patient plasma and 0.2 mL of thromboplastin/calcium chloride reagent. PTT was measured using 0.1 mL of plasma, 0.1 mL of activated partial thromboplastin, and 0.1 mL of calcium chloride. Current analyzers can perform the same tests using one-half or even one-quarter the traditional volumes of reagents and patient specimens. This promotes the use of smaller specimen volumes, especially from pediatric patients or those from whom specimens are difficult to draw, and further reduces reagent costs.
Open reagent systems. A variety of reagents from numerous distributors are available for coagulation testing, and laboratory directors want the flexibility of selecting the reagents that best suit their needs without being restricted in their choices by the analyzers being used. Recognizing that the ability to select reagents independently of the test system is a high priority, instrument manufacturers have responded by developing systems that provide optimal performance with alternative manufacturer’s reagents, provided that the reagents are compatible with the instrument’s methodology.
Reagent tracking. Many automated instruments keep records of reagent lot numbers and expiration dates, which makes it easier for the laboratory to maintain reagent integrity and comply with the regulatory requirements. Additional features often include on-board monitoring of reagent volumes with flagging systems to alert the operator when an insufficient volume of reagent is present in relation to the number of specimens programmed to be run. Reagent bar coding supports record keeping because it tracks reagent properties and enables the operator to load coagulometers without stopping specimen analyses.
Point-of-care (POC) devices are created using cutting-edge technologies, such as fluorescence microscopy, microfluidics, electrochemical sensing, and photoacoustic detection. POC instruments primarily gauge the optical, mechanical, and electrochemical aspects of blood clotting. It is projected that these technological advancements will accelerate the coagulation testing market size in the coming years.
POC tools are used to measure blood clotting’s optical, mechanical, and electrochemical components. These technical developments are anticipated to expedite the market expansion for coagulation testing.
POC coagulation testing is not new to the industry. It has been in use since 1966 in the setting of cardiac surgery, using the whole-blood activated clotting time (ACT) for heparin monitoring in the operating room. Today POC testing has expanded beyond ACT. The majority of POC devices are portable, allowing for close patient testing, bedside testing, self-testing, and newborn testing. Physicians and patients both value the conveniences of the equipment’s portability, small sample size, and immediate turnaround time for results.
For the identification of diseases, such as hemophilia, von Willebrand disease, and deep vein thrombosis, POC coagulation testing equipment are employed. POC coagulation testing equipment’s quick results help with the prompt detection and treatment of coagulation abnormalities.
POC testing may be extensively used in anticoagulation clinics. Patients on vitamin K antagonist oral anticoagulant treatment must be checked on every month. Anticoagulation clinics offer this service in an outpatient setting, utilizing a POC device for the prothrombin time/international normalized ratio (PT/INR) test. A quick test result minimizes patient waiting time, offers time for patient education, and permits dose modifications within the same clinic appointment.
The PTT and thrombin clotting time are further POC coagulation diagnostics, and new assays like fibrinogen are likely to become accessible in the future.
The market for POC coagulation testing equipment is anticipated to grow as a result of rising surgical operations, rising prevalence of coagulation diseases, and favorable reimbursement policies. However, it is anticipated that a scarcity of qualified professionals may impede industry expansion. By product, the market may be viewed as coagulation meters, coagulation reagents, and lancets. The segment of coagulation meters is further divided into tabletop and portable coagulation meters.
The POC coagulation testing equipment market is segmented into PT/INR, aPTT, and fibrinogen assays, based on test type. As these tests are used to track the effectiveness of anticoagulant medication like warfarin, the PT/INR testing market is anticipated to rise rapidly. The market players see growth opportunities with the development of new technologies like wireless devices and miniaturized devices.
According to the World Health Organization (WHO), prevalence of chronic diseases like cardiovascular diseases, cancer, and diabetes is increasing rapidly worldwide. These diseases require long-term treatment, which is expected to increase the demand for POC coagulation testing devices.
Next-generation POC. An advanced medical-grade ultrasonography technique is now used by a POC hemostasis device to evaluate the coagulation characteristics of a complete blood sample. The method enables medical professionals to provide coagulation therapy that is patient-centered, enhances care, and maximizes the use of blood products. It is the first whole-blood hemostasis testing device, especially approved for use in POC settings, such as operating rooms, emergency departments, and intensive care units. This is due to its quick results, simplicity of use, and dials screen for easy interpretation.
The recently introduced technologies are luminescent oxygen channeling immunoassay (LOCI), magnetic sensor-based POC coagulation testing, microfluidic strip-based POC, microresonators based on Microelectromechanical systems (MEMS) technologies, and electrochemical sensor-based coagulation testing. Along with these in-vitro techniques, Campbell et al. introduced laser scanning confocal microscopy (LSCM) to observe in-situ thrombin generation. Other in-vivo studies of thrombin introduced microenzyme immunoassay to measure thrombinantithrombin complex (TATc) levels.
But POC technologies are facing challenges, which include the quality, robustness, cost, intellectual property issues, regulatory approval, clinical acceptance, the economics of test usage and the ultimate market size. The stringent government regulations, and the high risk and costs associated with tests and treatments, which limit their usage to only the population that is economically capable, have a negative impact on the global coagulation testing market. Lack of skilled labor and higher cost of devices may affect global market growth. Several studies have declared that the test results at the central laboratories are more reliable than the tests by the POC coagulation testing (POCCT) devices, which further debates their attractiveness in the market. The POC testing devices market is also handicapped by lack of uniformity, relatively expensive devices, and lack of awareness.
Once you start moving POC into the hospital, it becomes more difficult. The workhorses like INR and PTT are costly to do at the POC – these are high-volume tests. Also, there are limitations, at least in the literature. For example, there is one instrument that measures PT/INR that has an electrochemical endpoint and it is completely insensitive to fibrinogen, so if a patient did not have any fibrinogen on the hospital floor, that PT/INR would indicate that the patient is normal. A lot of the PT/INR POC tests are indicated for warfarin monitoring only, so iti’s hard to know how those tests perform in an ICU, where there are many other considerations.
With Covid rearing its ugly head again, the D-dimer, one of the most important biomarkers for Covid-19 survival, one of the pandemic’s healthcare heroes in the coagulation tests, is gaining relevance again.
D-dimer is predictive of serious illness and death due to SARS-CoV-2 infection, and thereby provides further support for the notion that POC D-dimer testing might be a helpful tool for the early triaging of Covid-19 patients presenting to the hospital emergency department, and for monitoring patients during the first week of hospital admission. A number of subsequent studies conducted around the world have confirmed that D-dimer is elevated in those with severe Covid-19 and highest in those who are most critically ill and those who do not survive.
Coagulation has come a long way since Huang Ti, the Chinese emperor, first described the length of bleeding time around 3000 years ago. It was in the year 1628, when William Harvey scientifically proved blood circulation, and in 1905 the phenomenon of coagulation was first put forward by the German scientist Paul Morawitz. In 1960, the coagulation cascade was described, which led to the development of the first clotting time tests.
Rise in demand for disposable coagulation testing equipment is giving profitable business prospects in near future. Distribution channels are playing a key role in the growth of the coagulation testing industry. The disposable coagulation testing kit is commonly available at offline pharmacy stores. Meanwhile, the rise in e-commerce platforms is improving the visibility of the commodity. Cost-effectiveness and highly dependable kits are going to fuel market growth in the next year.
We are making strides with automation, and there are great assays coming out that help us take care of patients. The increase in cardiovascular diseases, a rise in the geriatric population, high demand for point-of-care coagulation testing, and technological advancements, such as faster and easy-to-use devices with advanced sensors technology, are providing the requisite impetus.
Moreover, new technology in coagulation testing is providing fuel to the growth of the market. Furthermore, rise in the prevalence of liver illness, thrombophilia, and hemophilia are anticipated to boost the coagulation testing market growth. The coagulation testing market share is expected to grow significantly with the increase in the prevalence of blood disorders. Moreover, an increase in expansion of healthcare infrastructure is one of the primary driving factors aiding the growth of the market.












