Industry
Beyond Covid-19

The pandemic, while taking a toll on providers and patients alike, enabled the discovery of deep reserves of resilience and innovation.
The Covid-19 pandemic permanently changed global healthcare, from accelerating the adoption of new technology and care delivery models to increasing the focus on sustainability and resiliency. At the same time, it accentuated existing workforce challenges and the global disparities of health equity.
With more than 70 percent of the world’s population having received at least one Covid-19 vaccine, the sector now faces critical questions that will shape its future in 2023 and beyond. In the coming year, healthcare providers, other sector participants, governments, and regulators must ask themselves how they can:
- Translate lessons about virtual health delivery during the pandemic into improved access and treatment.
- Leverage technology to reduce costs and demands on health workers while improving care for patients.
- Reduce their carbon footprint and thereby help to mitigate some of the environmental threats to public health.
- Ease the burdens on an increasingly stressed workforce by reshaping the scope of job requirements, allowing more remote work, and providing better support such as mental health services.
- Better prepare facilities, supply chains, and partnerships for future pandemics, public health events, or natural disasters.
Covid-19 has not disappeared from the global stage, but public health professionals are increasingly optimistic that the pandemic is becoming endemic, meaning that while the virus is still present, it is becoming more manageable and predictable — more like the seasonal flu.
While several hundred thousand new infections — and hundreds of deaths — were being reported daily worldwide at the end of 2022, new vaccines have reduced the number of deaths dramatically. During 2022, no new strains were declared a “variant of concern” by the World Health Organization.
Healthcare stakeholders should remain alert, nimble, flexible, and prepared for spikes and valleys in Covid-19 cases as well as other communicable diseases.
At the same time, Covid taught health professionals how to adapt to remote working, virtual doctor visits and shortages of medical supplies, personnel, and services. Indeed, the lasting impact of Covid-19 may be one of opportunity in which the health sector has a chance to reinvent itself and capitalize on trends that were emerging even before the pandemic, such as shifting consumer preferences, changes in patient behaviours, and rapidly evolving technology. The sector also should continue to explore clinical innovation and new care delivery models — some of which, like telemedicine, were successfully used on a widespread basis during the pandemic.
If the health sector takes advantage of these opportunities, it could transform care delivery, the patient experience, and ways of working at hospitals and other facilities, while also reducing inequities and boosting resiliency. Deloitte in a recently released report reviewed the five key areas that are critical to this transformation, virtual health delivery, digital transformation, health equity, workforce, and sustainability.
Understanding depths of digital transformation
Many countries are making progress in adopting EHRs. The NHS, for example, plans to adopt electronic health records (EHRs) at all hospitals and community practices in the UK by 2025.9 While this provides a strong digital backbone, the challenge in many countries is interoperability — getting related hospital systems to link with each other — and extending those connections to external services such as primary care centers.
In addition, the quality and comparability of the data is inconsistent. Unstructured or “dirty” patient data can provide an incomplete picture of a patient’s health. Most organizations are adopting standard data sets, building data “lakes” to combine data, and using the latest artificial intelligence (AI) tools to develop meaningful insights.
Despite this, in many countries, vital medical information is still stored on paper. When information or images are shared, it is often done by fax, mail, social messaging applications, or patients themselves, who carry their physical documents from one provider to the next.
The advent of Health Information Exchanges (HIEs), in which healthcare organizations can exchange electronic health information, is growing rapidly. New payment and reimbursement approaches are increasing the focus on care coordination. For example, HIEs can help providers avoid unnecessary readmissions and medication errors, improve diagnoses, and decrease duplicate testing.10 The exchanges are standardizing technology to allow providers and patients to connect more effectively and allow care to be distributed more broadly across multiple care pathways, care settings, and geographical regions.
Heading to the cloud
Financial pressures are a double-edged sword in the digital transformation of healthcare. On the one hand, technology can improve efficiency and reduce costs. On the other, the expense of moving systems to new digital platforms can slow the adoption of cloud solutions.
In the UK and Scandinavian countries, concerns about margin pressure are driving digitization, yet in the US and Australia we see margin preservation restricting the adoption of new technology. In response, pricing is becoming subscription- or usage- based and is moving from capital to operating expenditures. Deloitte, for example, has formed a partnership with Amazon Web Services (AWS) to use third-party data in the cloud to create an efficient, robust, and secure healthcare data ecosystem that can improve population health, reimbursement and provide other real-world insights.
Nevertheless, most health executives recognize the longer-term benefits of digitization. A survey of almost 400 health executives across six countries found that two-thirds of respondents expect to move their IT infrastructure to the cloud within a year, and 96 percent expect to do so within three years.
Much of the focus around digitization has been on operations — specifically, the managing and delivery of care — but, technology, and specifically automation, is also reducing costs and improving back-office processes such as clinical coding, billing, scheduling, payroll, and procurement.
Covid-19 accelerated the shift to cloud-based technologies designed to strengthen business operations and drive more customer interactions into the digital realm. This trend is forcing the large EHR providers to migrate their products and services to the cloud and develop partnerships with Customer Relationship Management (CRM) and Enterprise Resource. Planning (ERP) providers.
In June 2022, for example, Oracle completed its acquisition of Cerner with plans to expand Oracle’s cloud business in the hospital and health system market, both in the US and internationally. Oracle said the acquisition will enable it to provide a new generation of information to health professionals that will improve treatment decisions and patient outcomes while lower providers’ administrative workload, enhancing patient privacy and reducing costs.
CVS Health and Microsoft announced a new strategic alliance in December 2021 to develop innovative solutions that will help consumers improve their health. The collaboration is designed to allow CVS Health to provide a data-driven and personalized customer experience to clients.
Cigna began using the cloud platform from Majesco’s L&A Group for its supplemental health solutions product suite in July 2022 after partnering with Majesco a year earlier to accelerate its digital transformation.
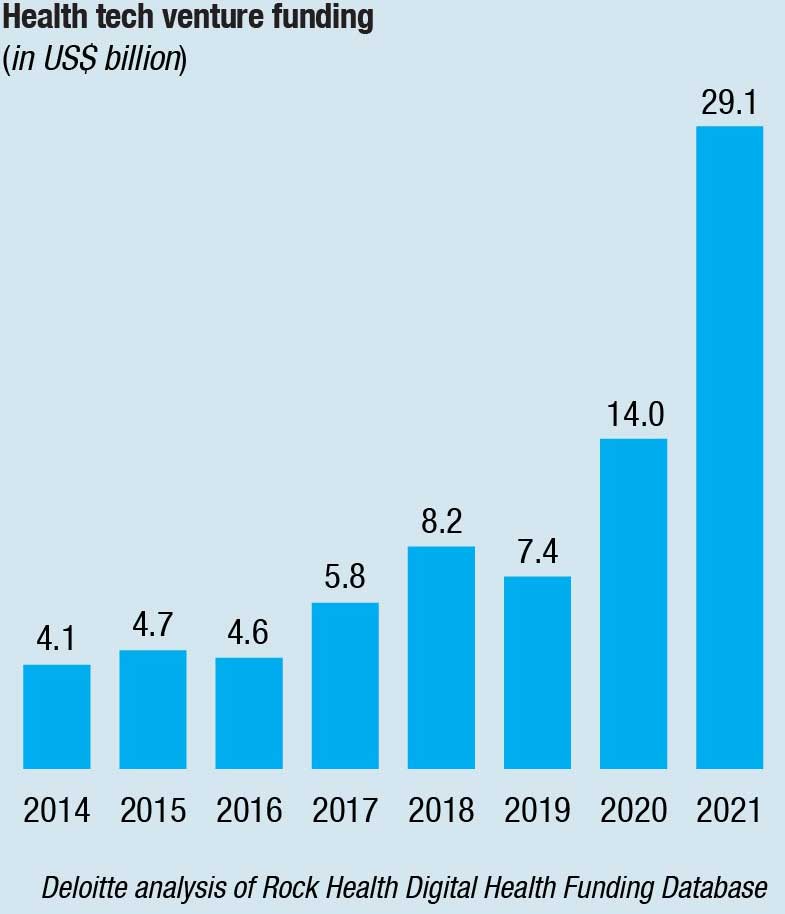
In addition, many venture capitalists, private equity firms, and healthcare organizations are investing in startup platforms. Globally, health-tech investments in 2021 topped USD 44 billion, double the previous year. Large tech-enabled platform companies could help hospitals and health systems improve efficiencies and scale quickly by modernizing existing systems and delivery models, addressing health-equity through a platform approach.
However, migrating to the cloud can raise environmental concerns. Some estimates show that cloud-based computing generates a larger carbon footprint than the airline industry—and that a single data center can consume as much energy as 50,000 homes. As more companies assess their indirect, or Scope 3, emissions, they must gauge the carbon footprints for partners, suppliers, vendors, and other third parties. AWS, Google Cloud, and Microsoft Azure all have introduced tools to help customers assess their carbon footprints and take steps to reduce them.
Emerging technologies
Emerging technologies such as AI, telehealth, blockchain, and monitoring devices, such as sensors, wearable and ingestibles, are providing real-time and continuous data about our health and our environment. This is redefining the future of healthcare and health delivery. Healthcare companies can use these innovations to provide more accurate diagnoses, deliver personalized treatment and predict risk or deterioration and intervene early.
Telehealth became widely accepted during the pandemic, and it continues to evolve, incorporating patient portals, telemedicine, mobile health, video conferencing, and remote patient monitoring. Already, patients are frequently using portals to schedule appointments and receive test results via their smartphones, and telehealth applications are expected to expand during the next five to 10 years.
Almost half of consumers said they attended at least one virtual medical appointment in 2021. While many cited avoiding Covid-19 as a primary reason for embracing the technology, they also found it more convenient because they could choose an appointment time that better fit their schedules. Ninety-two percent of those who used virtual appointments said they were satisfied with them, and 48 percent said they were very satisfied.
AI can work in conjunction with data such as EHRs stored on the cloud to develop a system of proactive continuous care designed to keep people well rather than episodic care delivered retrospectively when they are already sick. A new AI- empowered system at Johns Hopkins Health System scours medical records and clinical notes to identify patients who might be at risk of infection before symptoms develop. A study conducted by the health system found that patients are 20 percent less likely to die of sepsis because of the new tool.
AI4HealthCro, a not-for-profit public-private consortium based in Croatia, is developing AI technologies for the European Union that it estimates will free up as much as 1,944 man hours annually, save as many as 403,000 lives, and reduce healthcare costs by as much as €212.4 billion.
Not all health conditions or concerns require an in-person consultation with a clinical professional. AI is increasing patients’ options for receiving healthcare. Algorithms can diagnose and provide personalized advice and support to patients in automated channels such as call centers, text messaging, chat bots, and video consultations. According to Kaiser Permanente, 75 percent of enquiries are resolved in one visit using these remote channels.
One study, conducted in an urgent care setting in Sao Paulo, Brazil, during the pandemic, found that the implementation of an AI registration system cut down wait times by an average of 12 minutes and saved more than 2,500 hours a year in employee time.
AI already is being used to improve diagnostics and make predictive medicine more accurate. Researchers at Google’s DeepMind Health designed an AI algorithm that could identify factors for when someone was at risk for advanced kidney failure — and predict it 48 hours in advance. Overall, the algorithm had an accuracy rate of 55.8 percent, but in cases severe enough to later require dialysis, its prediction were accurate 90.2 percent of the time.
Whilst these new channels of advice and treatment have the potential to increase patient access, operate around the clock, and reduce the workload on already stretched clinical teams, careful testing and implementation is essential. The quality of the experience can be hampered by poor data quality, low data point counts, and lack of trained personnel for handling these technologies. Moreover, these channels must be synchronous so patients can move freely between them with one record being continuously updated and maintained. The risk is that often, when new technologies are added, they are implemented piecemeal rather that integrated throughout an organization or across a patient journey.26
Healthcare providers who use wearable technology to monitor chronic health conditions and to track vitals, sleep quality, and medications are finding the technology helpful. However, for large-scale adoption clinicians must agree on the parameters for alerts, appropriate clinical governance arrangements, and efficient work flows alongside effective reimbursement models for devices and data. Data accuracy and privacy, as well as cyberthreats, will also act as headwinds to adoption.
Health equity
Great disparities based on age, location, gender, income, race, ethnicity, religion, and sexual orientation persist in the global health ecosystem despite significant efforts to eliminate them by healthcare providers, insurers, government agencies, aid organizations, and others.
More than a quarter of the world’s population has no access to essential medicines, and for more than 2 billion people worldwide, medicines may be unaffordable, unavailable, inaccessible, or of poor or unregulated quality.
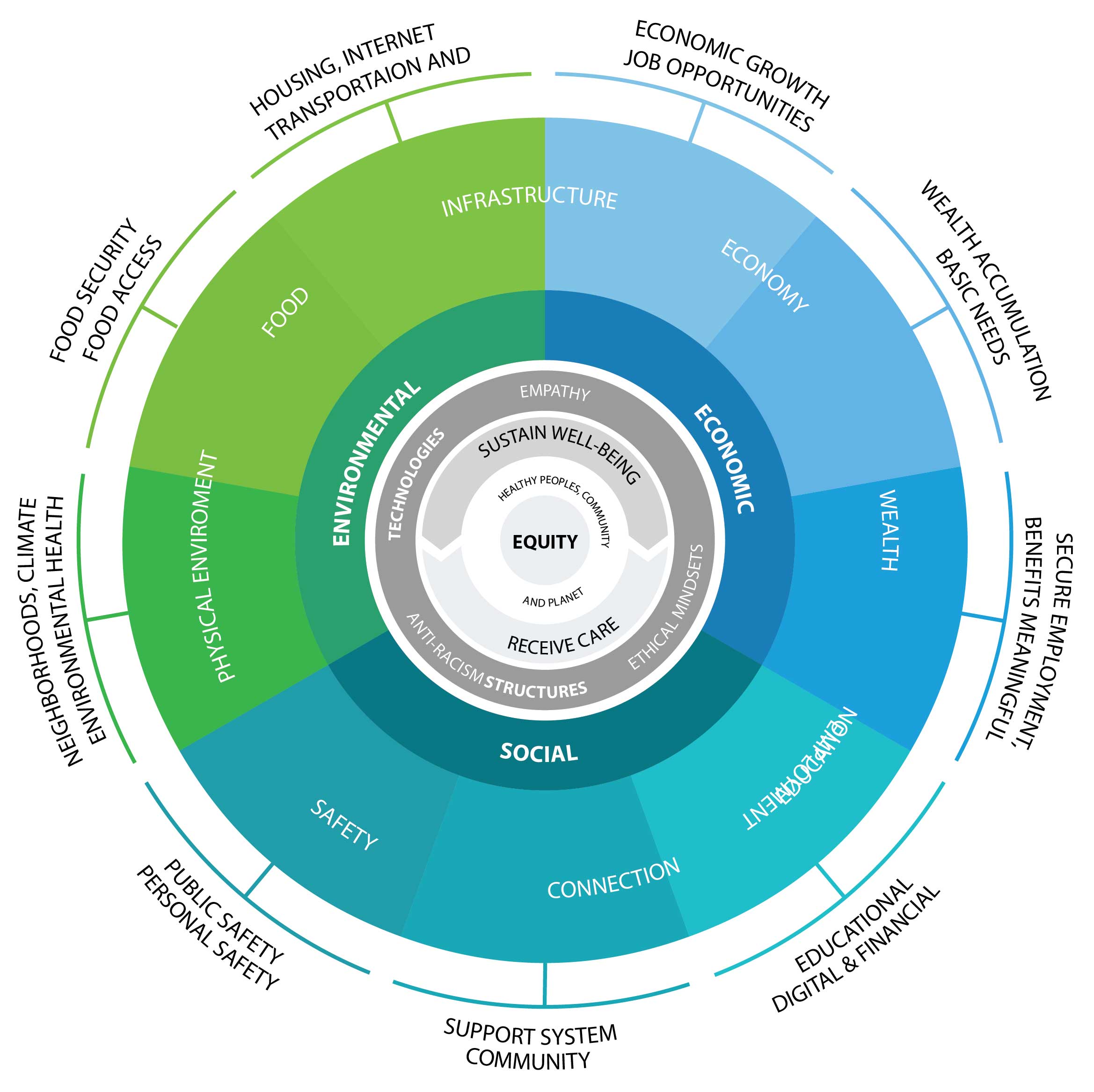
Social, economic, and environmental “drivers of health,” or social determinants of health, can have a greater impact on health outcomes than the care provided by clinicians — accounting for about 80 percent of health outcomes.2
The Covid-19 pandemic underscored the pervasiveness of health inequity. The virus disproportionally affected the most vulnerable groups, and focused public attention on how communities are only as strong as their most compromised members. As a result, many health organizations are rethinking how to address health inequity.
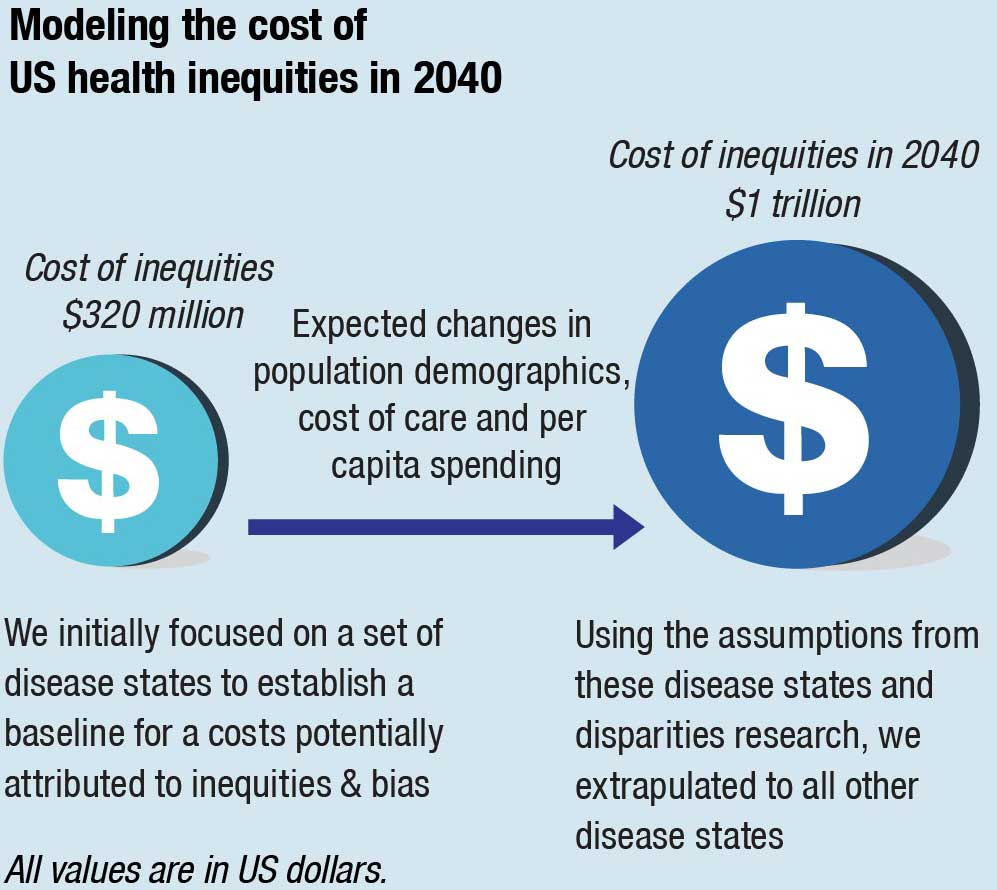
The cost of health inequities
Inequities across the health ecosystem limit underserved people’s access to affordable, high-quality care, create avoidable costs and financial waste that span society, and impact every individual’s potential to achieve health and well-being.
In the US health system, for example, inequities cost about USD 320 billion and could exceed USD 1 trillion in annual spending by 2040 if left unaddressed. This projected rise in healthcare spending could cost the average American at least USD 3,000 annually, up from current costs of USD 1,000 per year.
Meanwhile, the European Parliament estimated that health inequities in the European Union cost about 1.4 percent of GDP each year, almost matching defense spending of 1.6 percent of GDP.
Healthcare organizations can impact DOH for their patients and members, employee populations, and in their larger communities
The pressure to reduce costs
Globally, the healthcare sector is under pressure to reduce healthcare spending while increasing quality of care. Persistent health inequities have a substantial impact on health outcomes and spending. However, the industry hasn’t yet found systemic and sustainable solutions to address this complex challenge.
To address these disparities, health organizations must work outside of the traditional healthcare system and address the social, economic, and environmental factors that lead to healthy or unhealthy outcomes.
There is some light ahead. There are several global initiatives that are committed to making a change.
For example, Google is working with several healthcare organizations to develop a health equity tracker that can be used to create actionable, evidence-based policy changes to help disproportionately impacted communities receive equitable.
As companies develop products and services, invest in their communities, partner with others, and improve the diversity, equity, and inclusion of their workforce, they should consider designing for equitable health. This can help ensure the health and well-being of all individuals and provide access to affordable, high-quality care in all communities.
Addressing social and health equity is one of the greatest challenges of our time. We are in the midst of a social, political, and economic movement that can see the value and moral imperative to do so. Healthcare companies must take a leadership role and abide by the Hippocratic oath of “first do no harm.” However, only a coordinated effort among policy makers, industry executives, government officials, social influencers, and community organizers to close the widening global health equity gap.
Based on Deloitte report, 2023 Global Healthcare Outlook.












