Industry
Dedicated ventilator units may be the next thing in hospitals

Ventilation has been a life-saving treatment for seriously ill patients for many years. And more and more, hospitals overseas are incorporating dedicated ventilator units with multidisciplinary teams into their facilities.
Critical care has been an important aspect in patient care, and this has become evident during the Covid-19 pandemic, which was perhaps the greatest challenge seen in this lifetime. This has made the healthcare industry hugely resilient. If we look at the past three years, adaptability, collaboration, and innovation come to mind. Today, hospitals are also modified from the earlier established protocols during Covid-19 to provide resource-intensive care to patients besides providing routine hospital care.
Some countries in the presence of unforeseen Covid-19 pandemic have experienced lower total deaths, though higher numbers of Covid-19-related infections. Results here suggest that one of the explanations is the critical role of ventilator technology in clinical health environment to cope with the initial stage of Covid-19 pandemic crisis. These findings suggest that a forward-thinking and technology-oriented strategy in healthcare sector, based on investments in high-tech ventilator devices and other new medical technologies, can help clinicians deliver effective care and reduce negative effects of present and future respiratory infectious diseases, in particular when new drugs and appropriate treatments are missing in clinical environment to face unknown respiratory viral agents.
Having said that, long dependence on mechanical ventilation is an emerging health problem, especially after critical illness. Around 40 percent of patients entering the intensive care unit (ICU) require mechanical ventilation and 20 percent of these patients are expected to have increased ICU stays due to difficulty in weaning.
It has become vital to incorporate a multidisciplinary approach for patients receiving prolonged mechanical ventilation (PMV). Patients receiving PMV generally exceed the median length of stay in a hospital, and have a disproportionate readmission rate as compared to those ICU patients who do not require PMV. Typically, these patients are treated by a dedicated team within the ICU led by a pulmonologist who is responsible for making decisions and writing orders.
While a focus on the lungs is important when treating ventilated patients, moving to a multidisciplinary approach with respiratory therapists leading patient treatment, along with a dedicated team of physical therapists, occupational therapists, speech pathologists, acute care trained nurses, and dedicated case managers is suggested for future care models. This allows for more time with the patient, which enables early mobility and enhanced rehabilitation opportunities.
Studies show that a dedicated, multidisciplinary weaning unit for PMV patients not only reduces overall length of stay but also shows an improvement in patient survival, functional status, reduction in ventilator days or mechanical ventilation at discharge, and quality of life. This clearly illustrates an increased need for dedicated ventilator care units within the hospitals.
There are numerous reasons why patients are placed on ventilator care. Often, respiratory failure is secondary to the trauma that requires the use of PMV. That is why it is important to have a dedicated team who knows how to properly care for patients with varying primary health issues, including trauma, stroke and congenital heart failure.
Indian market dynamics
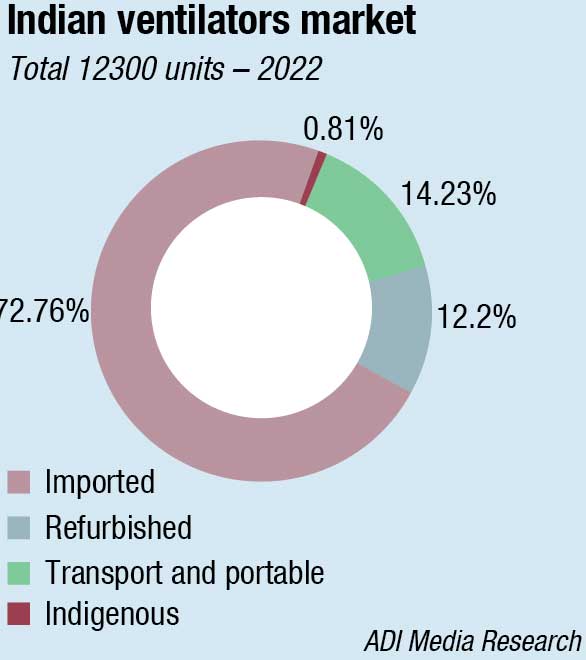
The Indian ventilators market in 2022 is estimated at 12300 units, valued at ₹813.5 crore. The imported ICU ventilators continue to dominate the segment with 83-percent share by value and a 73-percent share by volume.
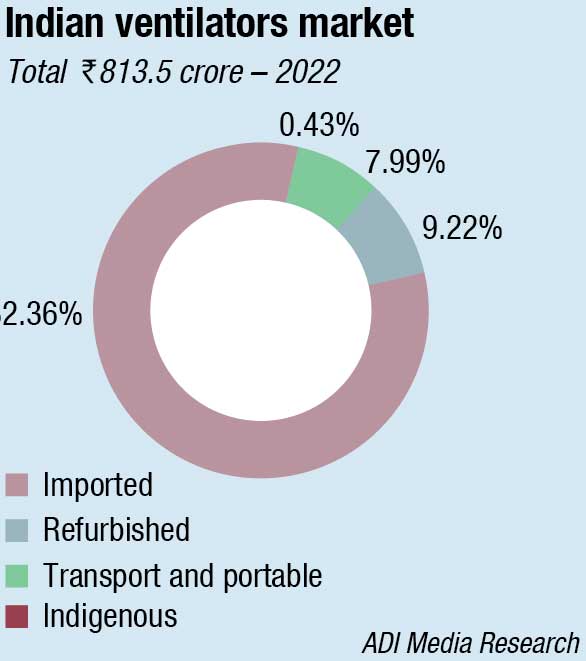
The refurbished ventilators are a dying category and are neither preferred by the buyer nor the authorities.
The indigenous ventilators are yet to make a serious comeback. The huge number of systems procured by the government in 2020 had kept public hospitals away in 2021. However, now bids are being invited again and along with the replacement market, the market is gradually calibrating and getting back to the pre-Covid level. The semi-urban sector is also looking up. Allied Medical and Skanray are the major vendors catering to this segment. Backed by its newly set up 200,000 sq. ft. of production floor space at Bhiwadi, a wider product range and a larger sales team, Allied Medical is gaining share steadily. The manufacturer is also one of the approved manufacturers to have qualified for the PLI scheme. The Make in India thrust has enabled offering a lower cost of ownership, a better control on after-sales service and spare parts.
In 2022, UVENT and Aeon Medical fared well, considering they were not there pre Covid. Three brands that had a setback in this segment are Philips, and to some extent Medtronic Covidien and Nihon Kohden. In June 2022, Philips Respironics, in line with the FDA regulation, had to recall all V60 and V60 Plus ventilators because an internal power fluctuation could cause the ventilator to shut down unintentionally, either with or without any visible or audible alarms. The power fluctuation caused a reboot of the backup alarm controller, which would lead to a complete shutdown of the ventilator without warning. Affected ventilators would cease ventilation either with or without alarms. Such failures led to patients being deprived of oxygen for an extended time, which could cause serious adverse health consequences and death, was the explanation. As of April 14, 2022, there had been reports of four injuries and one death associated with the use of the recalled devices. The recall targeted 49,680 V60 devices and 6991 V60 Plus devices for a total of 56,671 devices, manufactured and distributed between May 1, 2009, and December 22, 2021. Philips had already faced a recall of these models in March after it was discovered that some of the V60 and V60 Plus units were assembled with a faulty adhesive, leading to power failure.
|
Indian market for imported ventilators 2022 |
|||
| Leading brands | |||
| Tier I | Tier II | Tier III | Others |
| Draeger and Mindray | GE, Vyaire (IMT-Carefusion) and Getinge | Schiller, Hamilton, BPL and UVENT | Allied Medical, Air Liquide, and Aeon Medical. Philips, Nihon Kohden, and Medtronic Covidien. |
| *Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian ventilators market.
ADI Media Research |
|||
Global market scenario
The global market for mechanical ventilators is valued at USD 3.3 billion in 2022, and projected to record over 1-percent CAGR from 2023–2032. Of that, intensive care ventilators are predicted to reach USD 2.7 billion and adult ventilators USD 3.1 billion by 2032. The enormous patient pool with asthma and chronic obstructive pulmonary disease (COPD), along with the changing lifestyle, is increasing the deployment of adult ventilators. These units have in-built compressors, automated humidification, data monitoring, and invasive/non-invasive ventilation systems. These are extremely useful in complicated surgical procedures and treatment of chronic illnesses.
Invasive ventilation technology for mechanical ventilation generates some health problems as lung injury, alveolar overdistension that leads to inflammatory processes and fluid accumulation in lungs, ventilator-associated pneumonia etc.
Advanced ventilator technology
 Atul Jabde
Atul Jabde
Vice President – Ventilator Division,
Schiller Healthcare India Pvt. Ltd.
Ventilators have been a vital component of medical technology for decades, but recent advancements and emerging trends have led to a new era of highly advanced and efficient respiratory support devices. These innovations have not only improved patient outcomes, but have also led to increased efficiency and ease of use for medical professionals.
Another emerging trend in ventilator technology is the use of artificial intelligence (AI) and new algorithms which are beginning to receive interest. AI is assisting Clinical Decision Support Systems (CDSS) to deliver the correct evidence-based information to clinicians in the right format and at the right time. These technologies will enable ventilators to adapt to the patient’s unique respiratory patterns and adjust the ventilator settings accordingly. This can result in more precise and personalized treatment, leading to improved patient outcomes. Accurate predictive models to anticipate events, better decision support tools, and greater personalisation of care are becoming a quality standard. However, the major challenge remains with the ICU data integration in developing effective tools for AI. Big databases in all possible variables (e.g. physiologic, haemodynamic and demographic variables) are needed to develop CDSS for accurate prediction.
Additionally, many ventilators now come equipped with advanced sensors and monitoring systems. These sensors can detect changes in the patient’s respiratory and hemodynamic parameters and other important metrics. The data gathered from these sensors can be analysed in real-time to ensure the patient is receiving optimal treatment. Furthermore, the data can be stored and analysed over time to identify patterns and optimize treatment plans.
Finally, the use of 3D printing technology has revolutionized the production of ventilator components. This technology allows for the creation of highly customized and intricate components that are both lightweight and durable. This has not only reduced the production costs, but also enabled medical professionals to create unique components that are tailored to the patient’s needs.
In conclusion, the technological advancements have led to a new era of highly advanced and efficient respiratory support devices. As technology continues to advance, we can expect to see further improvements in ventilator technology that will continue to benefit patients and medical professionals alike.
The growth in the market is expected due to the packages of emergency relief accepted by governments around the world. Higher healthcare spending, developed healthcare infrastructure, demand for critical patient care, and new technological developments are some of the factors contributing to the growth of mechanical ventilator market.
Portable and transportable ventilators market is also witnessing a steady growth, and is the segment expected to grow with the highest CAGR till 2030.
Growing prevalence of chronic diseases like COPD, bronchitis, asthma, rise in geriatric population disorders, increasing level of pollution, changing lifestyles of people, and growing number of unintentional cases are driving the demand for ventilators. It is projected that the clinical benefits provided by mechanical ventilators for the diagnosis, treatment, and mitigation of chronic respiratory illnesses will boost equipment deployment.
Risks linked with ventilators as acute respiratory distress syndrome (ARDS), sepsis, ventilator-associated pneumonia (VAP), atelectasis, and pulmonary edema are common. Other risks associated with the use of medical ventilators include patient and physician resistance to technological transfer. Diseases, such as barotrauma, lung injury, pneumonia, and the high cost of medical ventilators, are some of the factors that are hampering the growth of the global market for ventilators. The lack of standardized nomenclature for various ventilation modes also limits the global market for ventilators.
To reduce these risks, companies are developing advanced equipment. Advancements emphasize the most urgent needs for improvement and most promising directions of future development. Mechanical ventilators are becoming more sophisticated, and expanding their application from the intensive care unit (ICU) to the respiratory medicine ward and even to patients’ homes for long-term treatments. Today, the evolution is rapid, with new devices and an increased number of ventilation modes and strategies being introduced to improve outcomes, patient-ventilator interaction, and patient care.
The technical performance in new ventilators has been improved manifold, and contributes to a better understanding of respiratory physiology and pathophysiology and of how different ventilation strategies interact with the respiratory system.
The future of ventilation technology
 Vysakh V.
Vysakh V.
Senior Design Engineer,
Skanray Technologies
The pandemic, increasing respiratory illnesses, a rise in geriatric patients, an increase in preterm births, and more, contributed to the ventilator market’s growth. Over the years, most clinicians and hospitals have relied on ventilators manufactured outside India. The expense of importing, its installation, availability of spares, and worldwide demand for ventilators during the pandemic have been a constant grievance in the medical community in India. Due to the increased demand for ventilators, hospitals are now looking at Indian manufacturers, who have excelled in building affordable invasive and non-invasive ventilators. Advanced microprocessor-controlled ventilation technology, in combination with the benefits of new innovative respiratory modes, has created opportunities to enhance patient care and quality of service.
Integration of volume capnogram, a graphical representation of exhaled carbon dioxide concentration over time, to ventilators has emerged as a valuable tool for assessing ventilation status, and helps in guiding clinical decision-making. Volume capnography is promising in diagnosing and monitoring pulmonary embolism, a potentially life-threatening condition. Also, this technology enables effective ventilation settings, ensuring optimal patient care.
Patient-ventilator synchrony is crucial for optimizing ventilatory performance, and aiding in patient recovery. Recent trends have focused on enhancing synchrony to minimize patient-ventilator asynchrony, promoting adequate respiratory support through advanced triggering and sensing mechanisms, and developing dual- or multi-level ventilation modes. These innovations improve coordination between the patient’s respiratory efforts and the ventilator’s assistance, enhancing patient comfort.
Auto-weaning is being viewed as a highly appreciated feature. Unlike the limited weaning facility of earlier machines, the advent of machine learning and faster processing power of systems, ventilators of today have built a capacity of self-learning to assist clinicians during their decision-making process.
The ongoing development of intelligent ventilation modes, the integration of artificial intelligence algorithms, and the utilization of biomarkers and predictive models hold promising potential for further improving patient outcomes and enhancing the delivery of ventilatory support.
Rise in the prevalence of lung and respiratory diseases among patients, such as COPD and bronchial asthma, which also causes postoperative complications after surgery and necessitates a consistent demand for high-frequency ventilators, and a surge in preterm birth rates across the world, is driving the growth of the global high-frequency ventilators (HFV) market.
HFV is considered a novel approach to mechanical breathing due to its capacity to deliver small, frequent breaths at high frequencies. In recent years, the usage of HFVs has accelerated, and they have been successfully applied in a variety of clinical settings, including new-born and adult intensive care units.
Studies have shown that low-tidal volume and low-pressure HFV can reduce ventilator-induced lung injury (VILI) in patients with ARDS. The application of non-invasive HFV in patients with acute respiratory failure is another development in HFV technology. This less invasive method has demonstrated potential improvements in oxygenation, a decreased need for intubation, and a shorter hospital stay. Another kind of HFV that is gaining priority in neonatal and pediatric intensive care units is high-frequency oscillatory ventilation (HFOV).
As per a report by Research Dive, the market for HFV is steady. It is expected to grow at a CAGR of 5.8 percent from 2022 to 2031. The reason for this growth is attributed to the increase in the prevalence of respiratory disorders, rising demand for advanced respiratory care devices, and advancement in technology. HFV has revolutionized the field of mechanical ventilation as it is a safer and more effective substitute for traditional mechanical ventilation. Recent technological advances have made HFV a promising therapy for people suffering from respiratory problems. It is anticipated that as the area of HFV advances, it will become increasingly important in the treatment of respiratory failure in seriously ill patients.
Mechanical ventilation continues to evolve
 Pradeesh CB
Pradeesh CB
National Prdt Manager – Critical Care & Anesthesia,
BPL Medical Technologies
Lately, technological advancements have happened in the field of mechanical ventilation for improved patient outcomes.
HFNC/HFOT is a non-invasive mode that gained attention during the pandemic. Non-invasive mask ventilation (NIV) involves oxygen delivery to the patient’s lungs without needing intubation, has become increasingly popular.
Closed-loop ventilation modes use advanced algorithms and AI to monitor a patient’s breathing patterns, automatically adjusting parameters based on changes in lung dynamics. This personalized ventilation approach minimizes caregiver inputs.
Modern ventilator features advanced ventilation modes that can even assist clinicians during CPR without disconnecting the ventilator from the patient. Remote diagnosis allows caregivers to monitor patients remotely.
Knowing the optimal ventilation setting is key to successful ventilation therapy. Modern ventilators provide more modes, parameters, and tools to help clinicians to go for lung-protective ventilation. Trans -pulmonary pressure measurement, lung recruitment with tools to determine the optimal PEEP, safe window, cuff pressure management to avoid VAP risks, EtCO2 and SPO2 monitoring, etc., are available in the market.
Weaning indicators, analyzers, parameters, and protocols have become a standard in most ICU ventilators that help clinicians determine a patient’s status in the weaning process and generate a dependable prognosis for their readiness for extubation.
VIT (ventilator integrated tomography) is an effective tool for lung imaging without the need for an X-ray. With VIT, continuous imaging of the lung function has become possible. By linking this technique with the measuring and control technology of intensive care ventilators, a wide range of clinical problems can be assessed, and appropriate therapeutic decisions can be made.
Many ventilators offer wireless connectivity, remote diagnosis, etc., allowing healthcare providers to monitor patients remotely and adjust ventilation settings in real-time.
Overall, the field of mechanical ventilation is constantly evolving, and technological advancements and emerging trends are improving patient outcomes and expanding access to care. Despite the technological advancements happening, the actual caregiving station is still the conventional way of ventilation being practiced.
In today’s ventilators, clinicians are looking for some distinctive features like reduced time spent on ventilators, simplified use of the device, and ability to integrate clinically useful information into the healthcare system, both directly and digitally. They foresee improved patient care as the main goal, along with the cost-saving feature.
Automation is another aspect through which clinicians can save their time and they do not have to be present at bedside all the time. In fact, a large proportion of the new solutions is software-based and allows automatic responses by the ventilators, typically within parameters that can be set and adjusted as determined by the clinicians. Europe and the US are both adopting automation and adapting to the new automatic protocols. However, complete automation is not yet on their list.
Clinicians can use help not only with ventilation adjustments but also with management of the data produced by the machine. It is no longer enough to be given numbers – clinicians want information. Automobile speedometer might be equivalent to waveforms and graphics, but new pictures can add 1000 words. Vendors offer graphic options on ventilators that give real-time feedback to help optimize device settings or incorporate color to enhance display identification.
Manufacturers have introduced a number of innovations to reduce alarm fatigue, a serious concern for many facilities. Some are designed to create fewer alarms, such as features that reduce leakage, others help to manage the alarms themselves. Smart alarms enable priority settings, graphical alarms provide visual information to indicate urgency, others send alerts remotely to better divide work among personnel.
Another innovation that has been making rounds is the ease of connectivity. Connectivity extends everywhere, not just within the facility. Covidien has launched its vital sync platform, which sends integrated ventilator data (as well as pulse oximeter and capnography data) to a central station or to any web-enabled mobile device, including laptops, tablets, and smartphones.
AML – Traversing ventilation strategies and technology
 Aditya Kohli
Aditya Kohli
CFO and Director – Sales,
Allied Medical Limited
Even though the concept of mechanical ventilation dates back to the 14th century, it was only in the last century that it was widely introduced into routine clinical practice. Since their initial appearance, mechanical ventilators have become more sophisticated, and have expanded their application from the ICU to the respiratory medicine ward, and even to patients’ homes for long-term treatments. This has been the result of combining the advances in our understanding of respiratory physiology, pathophysiology, and clinical management of patients together with technological progress in mechanical, electronic, and biomedical engineering. Nowadays, this evolution is still rapid, with new devices and an increased number of ventilation modes and strategies being introduced to improve outcomes, patient–ventilator interactions, and patient care. Engineering and organization continue to play a relevant role in this process, not only in improving the technical performance of the ventilators but also in contributing to a better understanding of respiratory physiology and pathophysiology, and of how different ventilation strategies interact with the respiratory system. Originally, the classification of these modes was relatively simple, with controlled ventilation modes being used when the ventilator was imposing its action to the patient and assisted ventilation modes used when the ventilator was supporting the breathing of the patient. Allied Medical Ltd. (AML), Research and Development team introduces a number of new modes of ventilation, incorporating decision support tool system helping clinicians to adjust the setting automatically.
Intuitive and simple user interface with quick operational readiness and automatic device check provides confidence in use, and reduces training time. A wide range of ventilation modes makes it suitable for various clinical requirements in NICUs. Simple user interface and effortless operation makes Allied Meditec Vista to be innate, and require minimum amount of training for the medical and nursing staff. The trend in the neonatal intensive care unit is to use non-invasive ventilation, whenever possible; invasive ventilation is still often necessary for supporting pre-term neonates with lung disease, so as an advantage Allied Meditec Vista provides non-invasive and invasive ventilation compatibility in all the modes of ventilation as a standard feature. It also offers some dedicated modes for neonates like TCPL and high-frequency ventilation (HFV).
Therefore, connectivity to access real-time data quickly helps clinicians to take immediate healthcare decisions, as well as long-term care decisions. To top it all, if the ventilator or software system provides this information automatically, without requiring clinicians’ analyses, it will be more beneficial. With the growing importance in technologies like machine learning, augmented reality, 5G, and digitization, the ventilator industry in the last three years alone has seen significant changes. However, not all innovations are equal, nor do they follow a constant upward trend. Instead, their evolution takes the form of an S-shaped curve that reflects their typical lifecycle from early emergence to accelerating adoption, before finally stabilizing and reaching maturity.
A key innovation that has been evident is the remotely monitored ventilators in artificial intelligence. Remote ventilator monitoring systems allow healthcare professionals to monitor patient’s vital signs and ventilator data from anywhere in the healthcare facility. These devices use software to adjust the settings remotely according to the requirement, thereby reducing risk of infection to the healthcare staff. According to GlobalData, there are 40+ companies, spanning technology vendors, established medical devices companies, and up-and-coming start-ups engaged in the development and application of remotely monitored ventilators.
In terms of application diversity, that measures the number of different applications identified for each relevant patent, Art Medical leads the pack, followed by Weinmann Emergency Medical Technology and Somne. By means of geographic reach, that refers to the number of different countries each relevant patent is registered in and reflects the breadth of geographic application intended, ranging from global to local, Hamilton Bonaduz held the top position, while Johnson & Johnson and Air Liquide are in second and third spots, respectively.
Easy integration of piezo valves for gas handling
 Thomas Kunert
Thomas Kunert
Product Manager LifeTech,
Festo SE & Co. KG
Extremely energy-saving, silent and without any heat build-up – piezo technology offers many benefits for efficient and precise gas handling in medical technology and laboratory automation. The biggest difference between piezo valves and proportional solenoid valves is the energy consumption, which is up to 95% lower. Up to now, it has not been possible to simply replace proportional solenoid valves since piezo technology needs voltages of up to 310 V and thus specific electronics. Now, however, there are simple solutions for this, which we will be presenting in this article.
Why piezo valves need voltages of up to 310 V
The principle of piezo technology cannot be compared with a solenoid valve. The core element is the piezo ceramics. When this is electrically charged, it creates a polarisation that causes the ceramic material to bend. The bending is proportional to the applied voltage and enables the flow rate or pressure to be regulated proportionally. The higher the voltage, the greater the flow rate. The current consumption curve is completely different than for a proportional solenoid valve, whose coil is permanently energised.
Controlling flow rate and pressure
The design of piezo valves is very simple. They consist of a housing with ports, with the nozzles injection moulded into it. The gas flows in or out through these nozzles. There are one or two benders – made from piezo ceramics – and above each of them a spring, which ensures the return action.
You will need a 2/2-way or 3/3-way valve, depending on whether you want to the control pressure or flow rate. A 2/2-way valve is a very easy way of controlling a flow rate. It has one bender and two ports. The more voltage is applied, the further it opens. A 3/3-way valve has three ports and two benders. A complete pressure regulation system can be set up with this compact solution.
Easily integrating piezo valves
Piezo valves do not operate using 12 V – they need special electronics. To make actuation much easier, Festo has developed piezo driver electronics in the shape of the new solution VAVE-P that has everything needed for piezo technology. Using piezo driver electronics means you only need 12 to 24 V to actuate the piezo valves.
Koninklijke Philips is one of the leading patent filers in the field of remotely monitored ventilators. Some other key patent filers in the field include ResMed, Medtronic, Baxter International and Fisher & Paykel Healthcare.
The other entries of a total 42 companies are Air Liquide, Art Medical, Asahi Kasei, Autonomous Healthcare, Becton Dickinson and Co, BMC Medical, CareFusion 207, DEKA Research and Development, Dragerwerk, Drive DeVilbiss Healthcare, eVent Medical, Fisher & Paykel Healthcare, Freespira, General Electric, Getinge, Hamilton Bonaduz, Johnson & Johnson, Loewenstein Medical Technology, Pneuma Respiratory, Senzime, Separation Design Group, Shenzhen Mindray Bio-Medical Electronics, Somne, Teijin, Teleflex, Terumo, Vyaire Medical, Weinmann Emergency Medical Technology, and Weinmann Geraete Fuer Medizin.
Remotely monitored ventilators ensure the safety, viability, performance, sustainability, and versatility required to meet the needs of various patients and caregivers. Remotely monitored ventilators have become the preferred choice for both patients and physicians due to the Covid-19 pandemic, and this trend is expected to continue as the pandemic has led to an unprecedented need for remote patient monitoring.
IntelliCycle Pro – An intelligible approach toward patient-ventilator synchrony
 Ankit Gupta
Ankit Gupta
Deputy Product Manager – Anaesthesia,
Mindray India
Patient ventilator asynchrony is a common concern for both invasive and non-invasive positive-pressure mechanical ventilated patients. It has been reported that as many as 24 percent of patients undergoing invasive mechanical ventilation in the intensive care unit (ICU) face severe asynchrony with an asynchrony index greater than 10 percent. Studies have shown that the high rate of asynchrony is associated with ineffective trigger, flow starvation, delay of cycle, and some other conditions as well.
Patient-ventilator interaction is of utmost importance in spontaneously breathing patients. To that end, the goal should be optimal patient-ventilator interaction, with a balance between patient inspiratory effort and ventilator triggering, between ventilatory demand and delivery of flow and tidal volume, and between interruption of patient inspiration and cycling of the device.
In general practice, the inspiratory trigger is set at a fixed positive flow or negative pressure. But such fixed settings may create several complications as constantly changing patient lung dynamics and leaks are not considered.
Identifying patient-ventilator asynchronies, using flow waveform analysis, is a very useful tool for clinicians. However, the clinicians can only adjust the triggers based on the previous breath and may not always be available near the bedside, and the patient’s condition can change from breath to breath. So real-time optimization is impossible to achieve with this conventional method.
To enhance patient-ventilator real-time synchrony, Mindray has developed an unprecedented technology known as Intellicycle Pro. The Intellicycle Pro is based on closed-loop analysis of respiratory mechanics and ventilator waveforms to enhance patient-ventilator synchrony. IntelliCycle Pro can automatically adjust parameters to improve synchrony in inspiratory and expiratory phases. This algorithm improves synchronization by detecting inspiratory effort and adjust the inspiratory pressure rise time and determines and adjusts appropriate expiratory termination sensitivity. Thus, Intellicycle Pro decreases the patient’s work of breathing and improves patient’s comfort. As this algorithm not only provides a better comfort for patient but also helps clinicians to achieve better results in terms of patient-ventilator synchrony in case of changing patient condition without manual intervention, this algorithm may get established as a symbol of an exceptionally user- and patient-friendly ventilator in near times.
A forward-thinking and technology-oriented strategy in healthcare sector, investments in high-tech ventilator devices and other new medical technologies, can help clinicians deliver effective care and reduce negative effects of present and future respiratory infectious diseases, when new drugs and appropriate treatments are missing in the clinical environment to face unknown respiratory viral agents.











