Patient Monitoring Equipment
Patient Monitoring Continues To Be The Backbone Of Healthcare
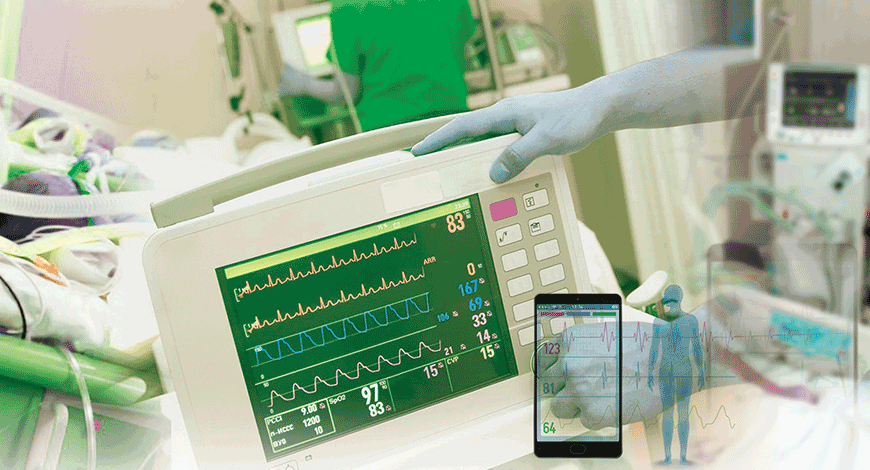
Design innovation in recent years has provided compact, lightweight, multi-purpose patient monitors that serve as a transport monitor, multi-parameter module, and/or a traditional bedside monitor – all-in-one device.
Healthcare providers are continuing to feel the pressure as the industry shifts to a value-based care model and the stressed importance of improved patient outcomes. In addition to the changing landscape, providers stay awake at night thinking about challenges like patient safety. And while the industry is making strides to address clinician pain points, issues such as lack of complete patient data and exhaustive alarm fatigue still remain. While challenges persist, there is an opportunity to improve and address the barriers that clinicians are currently facing with technology, which is why the patient monitoring market will continue to be on a steady growth path. The increasing number of patients in hospitals is making it difficult for doctors and nurses to monitor all the patients at the same time and this is one of the key factors driving the growth of patient monitoring system. Technological advancements in these systems are making it easier to use the equipment. The fact that the system helps doctors, nurses, and other hospital staffs to monitor the vital signs of patients on real-time basis is accelerating the adoption. Connected devices reduce the OpEx too.
Product innovation is one of the key strategies followed by manufacturers. Technology innovation in recent years has provided compact, lightweight, multi-purpose patient monitors that serve as a transport monitor, multi-parameter module, and a traditional bedside monitor, all-in-one device. These monitors move with the patient throughout their care path and provide uninterrupted data acquisition from patient to monitor to central station/EMR through seamless wi-fi and hardwired communications, easing clinical workflow and enabling a seamless medical record. Remote patient monitoring has now become a very useful advancement in the medical field. Not only is it cost effective keeping the chronically ill out of the hospital and more involved with their own health, but also by detecting early warning signs of any future complication which can arise. Wireless capabilities have also been a very functional advancement taking that usual image of someone on a hospital bed completely entangled in cables and giving that patient the ability to move around freely and to be more comfortable. Most equipment available now has similar functionality, including networking and integration compatibility, patient parameter availability, and ease-of-use for the staff (touchscreen, straight forward menus) to name a few. The next big wave of innovation looks to be coming from the telemedicine sector but that integration into mobile apps and wearable technology is still in its infancy.
Technological advances
New patient monitoring technology provides clinicians with smarter alarms and virtually gap-free data to lower the chances of preventable adverse events while helping them to improve patient outcomes.
Pulse oximetry. The World Health Organization recognized pulse oximetry (SpO2) as the most important lifesaving practice during surgery. This has driven a new era of patient safety during anesthesia and is recognized as the standard of care for the assessment of oxygenation, spanning virtually every domain of medical practice. Patient monitoring system manufacturers are continuously improving patient care by refining algorithms used in pulse oximetry. The upgraded technology is continuously pushed to devices via upgrades. The monitoring of SpO2 and advances in related technologies have improved patient care, providing critical information to enable the right care at the right time. An uptick in interest in CO2 monitoring in addition to traditional SpO2 is also being seen, as CO2 monitoring allows for more accurate assessment of patient deterioration. Hospitals are increasingly adopting these protocols to improve their ability to asses and respond to patient deterioration earlier.
Telemetry units. New wi-fi based patient monitoring system employs a wireless network to connect all of the patient information throughout the hospital. The system’s smart telemetry device keeps patients safe by acting as a stand-alone monitor when the patient is out of wireless range, with innovative back-fill capabilities that automatically synchronize all data once the patient is back within the coverage area. The device seamlessly connects to the central station, so patients are actively and continuously monitored, and all data goes to the hospital’s EMR. Latest monitors are focused on improving workflow by simplifying complex medical information, turning it into easily understood graphics, and maintaining complete patient records. The advanced monitors enable customization for specializations with ease. With two on-screen touches, any monitor is configured for the preferences of the specialist at hand. Continuity of care is critical as a patient moves throughout the hospital, so the transport monitors act as a full-color standalone touch-screen system, providing information on all major vital signs while a patient is moved to different care areas. Along with the advanced line of bedside patient monitors, the telemetry devices and their advanced embedded sensors, capture important patient data from the moment the patient enters the hospital to the moment they are discharged. That data is continuous and ready for care providers to review on all devices.
Alarm fatigue. Alarm fatigue is a constant battle for clinicians, as they are exposed to hundreds of alarms within an hour, and it is difficult for one clinician to respond to all these alarms at one time. In an effort to alleviate this concern, the industry is developing technology with smart alarms that alert the care team when a patient’s condition is changing. Early warning scoring (EWS) technologies navigate a number of real-time vital signs and produce a single score that alerts clinicians if a patient is showing signs of distress. By setting smarter alarm limits, clinicians can reduce false alarms, drastically decreasing the stress for both patients and staff, and respond to a single alarm to provide immediate, effective care to their patients. Mobility can further enhance the use of these technologies to improve clinician workflow. By allowing clinicians to access and respond to these alerts on the go, it can further support earlier response and intervention.
Pediatric and neonatal modes. A neonate is a critical care patient, but not at all like a little adult, so manufacturers are providing options for settings that are specific to neonates. A number of fetal monitors are available in the market, and the latest advancements provide expectant mothers with the ease of mobility through cable-less monitors. With this technology, mothers can move around freely during pregnancy and labor with continuous monitoring, improving their experience to walk, sleep, eat, and shower without the burden of being connected to multiple cables. The wireless monitor continuously feeds patient data to the EMR to provide complete coverage from first antepartum visit through labor, delivery, postpartum, discharge and follow-up visits.
In standard neonate mode, manufacturers are providing settings made to address lung and cardiac needs of the neonate—all master settings can be customized based on the hospital’s needs and standards of care. Thoughtful views pull together relevant information like OCRG (oxycardiorespirogram) with vital signs data so it can be simply visualized to inform care decisions. The alarm escalation features are very helpful in the NICU, as they can be customized to be based on specific numbers, percentages of values, time, warnings, and critical. For pediatrics, manufacturers continue the customization to accommodate different levels of patient needs at different stages in their lives. A number of different products are being developed specifically for pediatric measurements and comfort, like SpO2 for children and CO2 masks that are offered in various sizes for growing faces. The vital signs monitors feature a pediatric mode with custom algorithms for pediatrics and neonates, and they support the inputs required to establish a pediatric early warning scoring (PEWS) system.
Telemedicine and wearables. Telemedicine is the fastest growing segment in patient monitoring and is expected to continue to grow in the future. It is allowing care to be delivered outside the traditional hospital setting. For integrated monitoring outside of the hospital, clinical wearables can improve therapy adherence and chronic disease management by tracking vital signs and analyzing a patients’ health data as they advance in their treatment. This insight gives clinicians a deeper understanding of therapy adherence outside of the hospital, and can help them to make real-time adjustments to care plans. For patients suffering from chronic diseases, it’s important to evaluate their risk for developing a secondary health issue as a result of their pre-existing condition. Wearables can help track and analyze data to determine the risk of other complications, while helping the patient to manage their current chronic condition. By making adjustments to their care at home, patients are empowered to manage their conditions with the tools they need, which can improve therapy adherence and prevent hospital readmissions.
Road ahead
There will be a continued push for more monitoring outside the walls of the traditional hospital. Whether it’s urgent care, long-term care, or a hospital at home concept, there is a desire for care to be delivered in more places than ever before. In the patient’s home, it is anticipated that technology will enable monitoring to enhance care while simultaneously reducing the cost of care. Continued growth in monitoring customization will be seen in the future so that monitors quickly adapt to both the specialist and the patient. Overall, workflows are expected to become more streamlined, resulting in improved outcomes.
The healthcare industry will see the shift of medical wearables from the experimental phase to mainstream healthcare. There is interest in clinical-grade wearable devices and smarter data analysis tools for use in the hospital and at home. Wearables will become an integral part of the patient monitoring market, with the potential to address stress monitoring, blood glucose monitoring, and cardiac monitoring. There is potential for wearables to monitor otherwise undetectable behavior and physical changes in patients that could advance to a disease like Alzheimer’s, whose symptoms progress gradually over time. For the longer-term evolution of patient monitoring, Artificial Intelligence will continue to drive the technology for improved clinical decisions and the analysis of patient data.
Connected care technology with machine learning capabilities will empower clinicians to make proactive care decisions. By aiding clinicians with the most crucial data points at the time needed most, they have the opportunity to reduce unfavorable patient outcomes and improve patient care. As for patient data analysis, the industry is beginning to understand specific use cases for the immense amount of patient data collected by connected technologies, and much more specialization to improve patient care as a result of this data is expected in the next few years.












