Anesthesia Equipment
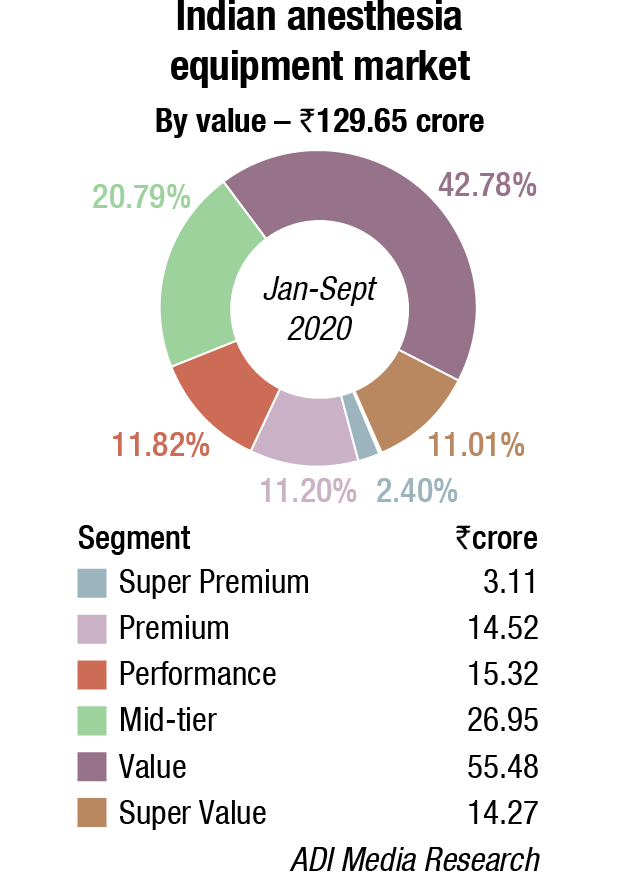
Anesthesia devices market received a major setback in 2020

With nonurgent surgeries on hold, the COVID-19 pandemic severely impacted demand for anesthesia instruments and reagents.
The practice of anesthesiology is inextricably dependent upon technology. Anesthetics were first made possible, then increasingly safe, and now more scalable and efficient in part due to advances in monitoring and delivery technology.
Consumer technology and telemedicine have exploded onto the scene of outpatient medicine, and perioperative management is no exception. Preoperative evaluations have been done via teleconference, and copious consumer-generated health data is available. Regulators have acknowledged the vast potential found in the transfer of consumer technology to medical practice, but issues of privacy, data ownership/security, and validity remain.
Inside the operating suite, monitoring has become less invasive, and clinical decision support systems are common. These technologies are susceptible to the garbage in, garbage out conundrum plaguing artificial intelligence, but they will improve as network latency decreases. Automation looms large in the future of anesthesiology as closed-loop anesthesia delivery systems are being tested in combination.
Moving forward, consumer health companies will search for applications of their technology, and loosely regulated health markets will see earlier adoption of next-generation technology. Innovations coming to anesthesia will need to account for human factors as the anesthesia provider is increasingly considered a component of the patient care apparatus.
 “Recent advances in anesthesia-related equipment have led to important improvements in monitoring technology. Availability of video laryngoscopes, extubation catheters, advanced supraglottic airway devices, and airway algorithms have been life-saving. Advances in perioperative technology include bedside ultrasonography, bispectral index monitoring, and advanced neuromuscular transmission monitoring systems. Ultrasound machines for bedside echocardiography, regional anesthesia, or central line placement now can be connected to a smartphone or tablet. These developments have proven to be game changers in difficult times.”
“Recent advances in anesthesia-related equipment have led to important improvements in monitoring technology. Availability of video laryngoscopes, extubation catheters, advanced supraglottic airway devices, and airway algorithms have been life-saving. Advances in perioperative technology include bedside ultrasonography, bispectral index monitoring, and advanced neuromuscular transmission monitoring systems. Ultrasound machines for bedside echocardiography, regional anesthesia, or central line placement now can be connected to a smartphone or tablet. These developments have proven to be game changers in difficult times.”
Divya Mulchandani, Consultant Anesthestist & ICU, SIDS Hospital & Research Centre
Global market
The global anesthesia machines market is expected to grow from USD 7.6 billion in 2019 to USD 9.4 billion in 2020 at a compound annual growth rate (CAGR) of 23.8 percent estimates The Business Research Company. The fact that COVID-19 is essentially a respiratory ailment has boosted the market growth. There is an increased demand for respiratory devices like ventilators, nebulizers, pulse oximeters and spirometers since oxygen therapy is a major intervention for patients with severe COVID-19 infection, and this factor is contributing to the market growth. In order to compensate for lack of ventilators due to the huge demand and short supply, hospitals have started to convert anesthesia machines into breathing machines. The market is then expected to grow at a CAGR of 8 percent from 2021 and reach USD 11 billion in 2023.
The use of computer-controlled anesthesia machines is an emerging trend in the anesthesia machines market. Computer-controlled anesthesia machines help in reducing the patient`s pain during surgical procedures and also provide features such as alarms to notify if case of an emergency or backup required to switch the defected pipeline or cylinder.
The integration of various functionalities, such as oxygen saturation level, carbon dioxide level, heart rate, and blood pressure, coupled with decision support systems and data analysis to aid clinicians to get better insights on their patients, is favoring the market growth. The introduction of new monitoring techniques, such as monitoring the depth of anesthesia, goal-directed fluid therapy, advanced neurological monitoring, improved alarm system, and technological advancements in objective pain assessment, is driving innovation in the industry. Decision support system (DSS) is another specialty of anesthesia. It is a digitized information receiver and relay center, which, in conjunction with anesthesia information management system (AIMS), helps the clinician in the delivery of health services, simultaneously monitoring the well-being of the patient. Thus, increasing investments which are supporting the technological advancements in anesthesia monitors, are having a major impact on the market’s growth, enabling faster deployment in the healthcare industry.
With the rising patient awareness levels and high prevalence of diseases and a rising number of surgeries, few other smaller players are expected to enter into the market in the coming years. Some of the major players of the market include B. Braun Melsungen AG, Medtronic PLC, Draegerwerk AG, Koninklijke Philips NV, and Fisher & Paykel Healthcare, among others.
Recent advances
Equipment used to perform any task, even complicated tasks like providing an anesthetic, can be described along a spectrum from tooling to automation. A tool is powered directly by its user, whereas a machine augments its user’s input via some external power source but remains directly under user control. The hallmark of automation is the ability of a machine to alter its function without direct user input but in pursuit of a user-defined objective.
Anesthesiologists used mostly tools and machines at the end of the 20th century. As the 21st century dawned, automated anesthetics became increasingly prevalent. The closed-loop anesthesia delivery system (CLADS) relies on a completed or closed feedback loop. Briefly, an automated device (for example, a ventilator) must be trained to a goal (for example, end-tidal carbon dioxide level) and govern an input that affects that goal. The causal interdependence of these factors is the closed loop. The common cruise control found in most automobiles is a simple closed-loop system receiving speed as its input and adjusting engine power to achieve a driver-set speed target. As when a car is being driven with the cruise control disengaged, the intraoperative warrant of an anesthetic provider is to make decisions based on data and implement changes. In the US, no truly automated CLADS is approved for commercial clinical use. Still, anesthetic workstations, infusion pumps, and monitors have progressed as increasingly intricate machines that ultimately leave the feedback loop open for the anesthesia provider to close themselves. Outside the US, automated CLADSs are employed in research and increasingly in clinical practice. These systems were first developed separately for specific parameters (for example, processed EEG monitoring, hemodynamic goals, and fluid resuscitation) and have been assessed in specific clinical scenarios, including in patient populations with relatively high comorbidity. In broader populations, the safety of these systems has been reviewed extensively. Automated anesthetic systems incorporating independent closed-loops for hypnosis, analgesia, and fluid management are undergoing feasibility studies. In one multicenter randomized controlled trial of parallel CLADSs using propofol and fentanyl, targeted to the proprietary bispectral index (BIS) and heart rate, the CLADS maintained significantly tighter control than manual operation over BIS (P <0.0001) and heart rate within 25 percent of baseline (P <0.0031). Inter-center variation among these parameters was minimal with automation (P=0.94) and significant with manual control (P <0.001). CLADS controlled total intravenous anesthetic (TIVA) infusions have also been shown to more tightly regulate depth of anesthesia, shorten recovery time, and reduce sedative agent consumption when compared with standard practice in a meta-analysis. Neurocognitive recovery, a measure of clinical importance beyond the perioperative period, might also be improved under automated TIVA administration. Pediatric applications are also developing. The February 2020 issue of Anesthesiology featured an editorial Robots will Perform Anesthesia in the Near Future. In some markets, automatic administration of volatile anesthetics via closed-loop titration is commercially available. It is expected that automation will increase rapidly, becoming the norm in the operating room in the next 10 years.
Monitoring beyond the operating room. The pursuit of new and more valuable patient data extends beyond the intraoperative setting. Consumer technology companies have poured resources into the developing consumer healthcare market. The Consumer Electronics Show (CES), the preeminent trade show in the US for all things tech, now sees regular entries from consumer healthcare technology seeking clinical application. Augmented reality technology from the video-gaming industry, for example, has made its way into the intensive care unit (ICU) to quantify patient mobility. Wireless technologies with low latency and ever-improving stability, developed for the consumer, may someday untangle anesthesiology workstations.
Telemedicine, a natural by-product of advanced videoconference products in the consumer space, and its application to the perioperative surgical home model of care constitute perhaps the clearest current example of consumer technology revolutionizing anesthesia practice. Small high-resolution cameras, microphones, and broadband data connections necessary for telemedicine have their origins in commerce and espionage. Their use in preoperative examinations, remote ICU care, intraoperative monitoring, and postoperative assessments is reviewed in detail elsewhere. Data security in consumer healthcare technology remains a challenge, but potential financial savings and sustained patient satisfaction continue to drive the expansion of telemedicine.
Innovation landscape technology. In 2007, Institute for Healthcare Improvement (IHI) began recruiting organizations from around the world to participate in a collaborative to implement what became known as the Triple Aim. Researchers described the Triple Aim as simultaneously improving the individual experience of care; improving the health of populations; and reducing the per capita costs of care for populations. IHI and its close colleagues had determined that both individual and societal changes were needed.
The Triple Aim of healthcare was launched in 2008 and has since guided many efforts in healthcare development. While chasing improved outcomes at a lower cost for more patients, technology enjoys several advantages over the traditional pipeline of medical innovation.
Bottom-up innovation and so-called solution shopping are common: technology often makes a task or measurement possible before its clinical use, or even its clinical need, is clear. Famously, smart watches and fitness trackers introduced essentially continuous activity and heart rate monitoring, earning applause from society at large and market success. Less developed healthcare systems may embrace this technology before advanced systems with pre-existing viable alternatives, leading to a leapfrog effect wherein nascent technology proves its validity in developing systems before adoption in advanced healthcare settings. Today, clinicians in advanced healthcare delivery systems remain faced with uncertain accuracy and reliability of consumer-grade medical information and have yet to codify its use in clinical care.
The fields of psychology, economics, and behavioral science will guide the implementation of the ever-increasing quantities of available patient information. Accounting for human factors and social engineering preserves the anesthesia provider’s most valuable resources: time and attention. Automated systems must be paired with an understanding of human operator behavior if they are truly going to improve care. Even if implemented with the strongest multi-disciplinary evidence supporting a technology’s utility, use will vary as the discrepancy between evidence and practice continues.
Development costs and regulation persist as necessary barriers to innovation. Development costs for novel technology continue to climb in step with the intricacy of products proposed and must be counteracted in the price of implementation. Regulation continues to function as a basic quality-control measure at the societal level. Markets employ varying standards for the evidence behind new medical technology, but new regulatory pathways aimed at bridging the gap between medical and consumer technology may smooth this process. The US Food and Drug Administration has acknowledged the value of technology transfer between medical and consumer realms, most recently by presenting Demystifying Regulation at the CES in January 2020 in an attempt to aid tech startups navigating a complex regulatory framework.
Although some impedance to innovation can be found in prudent quality assurance, philosophical opposition to change is a human habit borne out over centuries with real impact. Technological advance in anesthesiology is an uneasy topic for many practitioners. With innovations, practitioners can perceive a threat to their purpose and professional identity, perhaps even the reasons for which they dedicated their careers to the service of humanity. Institutions with a vested interest in the status quo (manufacturers, training institutions, and providers) often perceive a threat to power, influence, or prosperity in the face of sweeping change. In his last book, Innovation and its Enemies, the late director of the Harvard Kennedy School’s Science Technology and Globalization Project, Calestous Juma, details examples of this preservation instinct combatting waves of technology that upended certain sectors of society. Coffee was banned centuries ago as a substance that encouraged communal gathering and the exchange of ideas. Margarine, a threat to butter sales, was legally required to be dyed a painfully bright shade of pink. Resistance to innovation sometimes leverages coercive force (for example, law) to preserve a way of life, work, or thought. Still, today the café is ubiquitous and selling yellow margarine is not a crime. Anesthesiology’s experience with automation is already complex and under way. Embracing this wave and responsibly ushering it forward constitute the best way to avoid own pink margarine legacy.
Future is already here
As William Gibson famously began to note in the mid 1990’s, The future is already here – It’s just not very evenly distributed. The delivery of anesthesia, its preoperative assessments, and postoperative care vary by health system, resource setting, and society. However, the trends toward automation, non-invasive monitoring, remote monitoring and management, and CDS enabled by AI and improved information technology infrastructure are clear in our field. Each health system, in its setting, will continue to pursue improved outcomes for more patients while expending fewer resources in accordance with the triple aim. Inter-system variation will lead to leapfrog innovation where a set of advances more quickly enacted in one setting will provide the experience used to justify their implementation elsewhere.
Specifically, the CLADS is a mature technology that provides tight control of measurable variables during an anesthetic, but further study is necessary to elucidate clinical relevance (neurocognitive dysfunction aside). Monitoring has become increasingly non-invasive and processing-dependent as we extract novel metrics from proprietary combinations of existing metrics. Telemedicine has the potential to revolutionize the perioperative surgical home model of care and serves as a vanguard for the adoption of consumer-grade technology (telecommunication or otherwise) by medical fields.
Along with technological innovation, social engineering, and the constructs of efficient business will help increase quality and value in anesthesia care. Increasingly intricate synthesis of the incredible quantity and breadth of health system and patient metrics will inform this process. Behavioral science and economics will additionally guide the implementation of CDS systems, underpinned by the technologies noted above, with the aims of mitigating provider fatigue and minimizing errors.
Innovation in anesthesiology continues to be driven by the triple aim of healthcare for the benefit of patients and society. Parts of the trends discussed are inevitable results of economic and social forces acting upon the medical field. An informed and alert profession can shape the coming age and guide its members to meaningful and impactful practice. The future is here, and engagement with innovation will determine share of its prosperity.











