Defibrilators
The evolution of technology continues
With more advanced detection algorithms, the potential integration with leadless pacing, and the possibility to serve as a remote monitoring device to recognize atrial fibrillation, acute ischemia, or electrolyte imbalance, the application of ICDs is rapidly evolving.
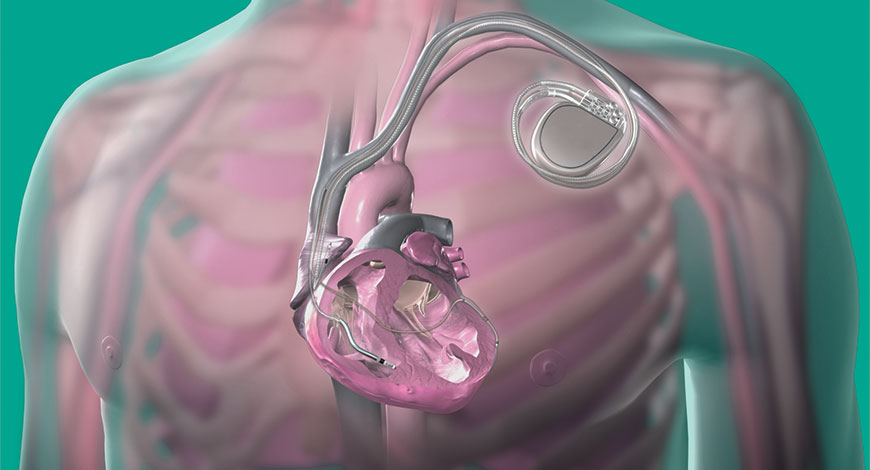
Modern cardiology develops and progresses through innovations in technology and a deeper understanding of the pathophysiology of heart diseases. Indeed, marked advances have been made since 1958, when the first pacemaker was implanted. Since their formal introduction in 1980, implantable cardioverter defibrillators (ICDs) have undergone innumerable design modifications through several generations. They are indispensable today in successfully managing fatal ventricular arrhythmias. Their role in averting sudden cardiac death is recognized beyond doubt. Their applications and indications have continuously expanded over the last two decades. This article reviews the salient features in the evolution of ICDs, their current indications, recent advances and future directions. With more advanced detection algorithms, the potential integration with leadless pacing, and the possibility to serve as a remote monitoring device to recognize atrial fibrillation, acute ischemia, or electrolyte imbalance, the application of ICDs is rapidly evolving.
Despite the growth and widespread adoption of ICD technology, important unsolved problems remain. These include implant-related complications, intravascular infections, structural failure, and risks of transvenous lead extraction. Considerable effort has been devoted both to reducing complications from transvenous systems and to developing extravascular ICD systems utilizing subcutaneous (S-ICD) or substernal (EV-ICD) electrodes. These can be used as stand-alone systems or potentially as part of hybrid modular systems combining extravascular ICDs with leadless cardiac pacemakers (LCPs).
 Dr Vineet Sankhla
Dr Vineet Sankhla
Consultant Interventional Cardiologist,
CIMS Hospital
“The external defibrillators have come a long way from large-sized manually operated devices to current portable AED and wearable cardioverter and defibrillator. AEDs are an important part of the advanced cardiac life support system for the treatment of sudden cardiac arrest. They are designed to be operated by a layman during an out-of-hospital cardiac arrest. Apart from automatic analysis of the cardiac rhythm and delivering appropriate therapy, today’s defibrillator-monitor also offers additional features of vital signs assessment like temperature, BP, 12 lead ECG, and wireless transmission of the waveforms to hospital ahead of patient arrival, SpO2, carbon monoxide, and methemoglobin monitoring. They are also capable of giving audible CPR instructions and delivering higher energy to 360J. The can be used by both emergency medical personals and code-blue medical team of hospitals. Modern AEDs are made to meet the special needs of air-medical and defense operations also”
As major improvements over the early devices, the second generation ICDs were designed to detect ventricular arrhythmias (VA) using a probability density parameter based on the concept that, unlike sinus rhythm, ventricular fibrillation did not maintain an isoelectric baseline. This enabled bradycardia pacing ability and they were minimally programmable. This ended the need for separate pacemakers.
The second generation ICDs could do away with thoracotomy by the introduction of transvenous leads in 1988, which enabled the implantation procedure to be performed in an electrophysiology laboratory rather than open surgery. Furthermore, these devices possessed limited telemetry function to test battery strength, for which an external monitoring device was needed. Cylindrical aluminium electrolytic capacitors and silver vanadium pentoxide batteries of the first generation ICDs were replaced by lithium-silver vanadium manganese oxide batteries, which resulted in longer life of ICDs.
The first third generation ICDs were introduced in the early 1990s. Anti-tachycardia pacing (ATP), low energy shocks for terminating VTs, high level of programmability and telemetry functions were the key upgrades. To improve specificity in discriminating between VT or supraventricular tachycardia, various algorithms were developed. ICDs could be programmed into three different cycle length-related zones and the discriminative detection algorithms programmable in the two lowest zones. The highest programmable zone is meant for detection of fast VT or VF without any further discrimination to avoid unnecessary delay of delivery of therapy. Additionally, improvements were made in lead construction. The coaxial lead design of the first and second generation ICDs was replaced with the multi-lumen lead design in third generation ICDs. The coaxial lead had a layered design comprising a tip conductor, ring conductor, defibrillation conductor and an insulation layer between each conductor. The multi-lumen lead construction is based on parallel running conductors through a single insulating body. The key advantage of multi-lumen over coaxial leads is the fact that more conductors would fit into overall smaller leads. The tip and ring conductors are used for pacing and sensing, a defibrillation conductor for the coil located in the right ventricle and a defibrillation conductor for the coil located in the superior vena cava. The insulating body contains extra lumens to increase the lead’s resistance to compression forces.
 Dr Harshal Lahoti
Dr Harshal Lahoti
Consultant Interventional Cardiologist,
MGM New Bombay Hospital
“For life threatening arrhythmias, early defibrillation is the most crucial link in the chain of survival. Defibrillators can be classified into manual external defibrillators, AEDs, implantable cardiac defibrillators and external wearable defibrillators. Implantable cardiac defibrillators are akin to a pacemaker and implanted permanently in individual patients at risk of life threatening arrhythmias. Manual external defibrillators technically, have three important components: a power supply, capacitor, and inductor. There are two types of current delivery systems: monophonic and biphasic. Biphasic defibrillators are more effective and energy efficient thus less injurious. Devices that have dual power supply importantly permit portability”
ICDs of today or the fourth generation ICDs have progressively become smaller and more sophisticated. They weigh not more than 80–90 g and have a volume of 30 ml, measuring less than a centimeter in thickness. Newer lithium silver vanadium batteries now last up to 9 years. All modern ICDs carry the ability of overdrive pacing, i.e. ATP, which can often terminate VTs without resorting to shock therapy. In addition, ICDs are also available with biventricular pacing (cardiac resynchronization therapy) to improve symptoms in patients with advanced cardiac failure.
ICDs will continue to evolve, become even more tiny, equipped with more advanced detection algorithms to treat life-threatening arrhythmias. The potential integration of S-ICDs with leadless pacing may make this therapy suitable for a larger target population at high risk of SCD. Moreover, if the leadless pacemaker is epicardial, left atrial, and left ventricular pacing can be introduced and linked to S-ICD; alternatively application of a left ventricular seed would permit resynchronization. S-ICDs may also serve as a remote monitoring device to recognize atrial fibrillation, acute ischemia, or electrolyte imbalance.
New ICD and CRT-D devices such as the new Gallant from Abbott have received the CE Mark recently in February 2020. This new system pairs with the secure myMerlinPulse mobile app to help streamline communication and increase engagement between doctors and their patients. This sort of app-based ICD system which would allow patients to engage more frequently with their healthcare team by providing access to transmission history and device performance and schedule their appointments could be the immediate future of ICDs.
Application and refinements of global positioning systems (GPS) may allow remote monitoring and programming of pacemakers wherever patients are on the planet. Furthermore, these developments are ideal in rural and inaccessible areas. Incorporation of advanced technologies such as Artificial Intelligence (AI) in CRM devices will further help patients monitor their cardiac health by notifying them and their physicians in case of abnormal activity. These cutting edge technologies come with cybersecurity threats and would therefore require the latest cybersecurity controls and partnering with industry cybersecurity experts to provide input into the design and testing of these controls to provide a seamless and a secure experience.
Prediction and prevention of VT and VF is one of the greatest unmet needs in clinical electrophysiology. This need takes two forms, accurate stratification of long-term risk to select patients who will benefit from ICD therapy and short-term prediction of imminent risk both to warn patients and – potentially – to initiate ICD-based preventive therapies.
Prediction and prevention of VT/VF is the Holy Grail of device-based therapy to prevent arrhythmic death. Accurate prediction is the critical enabling step. Not only would it permit ICDs to warn patients or other devices to intervene but it would also permit investigators to assess the outcome of therapeutic interventions based on predictive algorithms. Such algorithms can be evaluated most efficiently in groups of patients at high risk, to ensure sufficient events in a control group. Conceptually, ICDs can measure atrial or ventricular intervals, EGM characteristics, or other signals unrelated to basic ICD function. Both interval-based surrogate measures of autonomic function and EGM measures of repolarization dynamics have been evaluated as candidates for short-term prediction.
Extensive evidence indicates that the autonomic nervous system is an important trigger for VT/VF in many patients. ICDs have the capacity to measure multiple noninvasive electrical surrogates of autonomic nervous system activity including resting sinus rate and beat-to-beat heart rate variability (HRV). Device-based measures of autonomic surrogates have had limited success in predicting heart failure hospitalization and mortality but have not demonstrated specificity in predicting VT/VF.
Even accurate prediction limited to specific subgroups of ICD recipients or specific high-risk conditions could be clinically useful. Despite these opportunities, the challenge is great because a useful prediction algorithm must operate continuously and thus require minimal power. Further, it must operate with extraordinary specificity.
Pacing algorithms comprise the ICD’s most obvious tool for preventive intervention. Both inappropriate and apparently appropriate bradycardia pacing are associated with the initiation of VT/VF, often through short-long-short cycles. Future ICD algorithms that recognize potential, pacing-induced VT/VF and respond with altered pacing may be an initial application, partially analogous to dual-chamber pacing algorithms for endless-loop tachycardia. Future closed-loop pacing algorithms could be designed to stabilize repolarization alternans and/or variability. Although it would add an additional level of complexity, preventive algorithms could be used to trigger separate implanted devices, including one of a variety of neural stimulators. To date, such approaches remain aspirational, as few pivotal studies have been performed and the primary focus of neurostimulation has been the treatment of heart failure.
ICDs have come a long way since their first implantation in humans in 1980, firmly cementing their place in preventing SCD. Despite four decades of continual design improvements and upgrades, ICDs continue to evolve and current research is ongoing to refine the ever expanding indications for their use. With time, it is hoped that these devices will become more cost effective and safer.












