MB Stories
Anesthesia workstations – Relentless technological transformation

The realm of anesthetic equipment is undergoing a transformative phase, with a pronounced focus on technological advancements that redefine the landscape of respiratory support.
Anesthesia is an ever-evolving field, with new techniques, technology, trends, and practices constantly emerging. In the ever-evolving landscape of modern medicine, the role of anesthetic equipment has taken center stage, ushering in a transformative era driven by cutting-edge technology. The essence of this journey lies in the pivotal position assumed by advanced anesthetic equipment, a key player shaping the landscape of medical care. The recent advancements, regulatory guidance, and the dynamic technological developments define the current state of anesthetic equipment. Innovation is no longer a choice but a necessity, with the potential to enhance medical care and redefine the standards of patient well-being.
Indian market dynamics
The Indian anesthesia equipment market in 2023 is estimated at ₹485 crore, and 5600 machines. The very-high-end, top-of-the-line models met niche demand with Draeger dominating the segment. A couple of other brands sold 1–2 machines each.
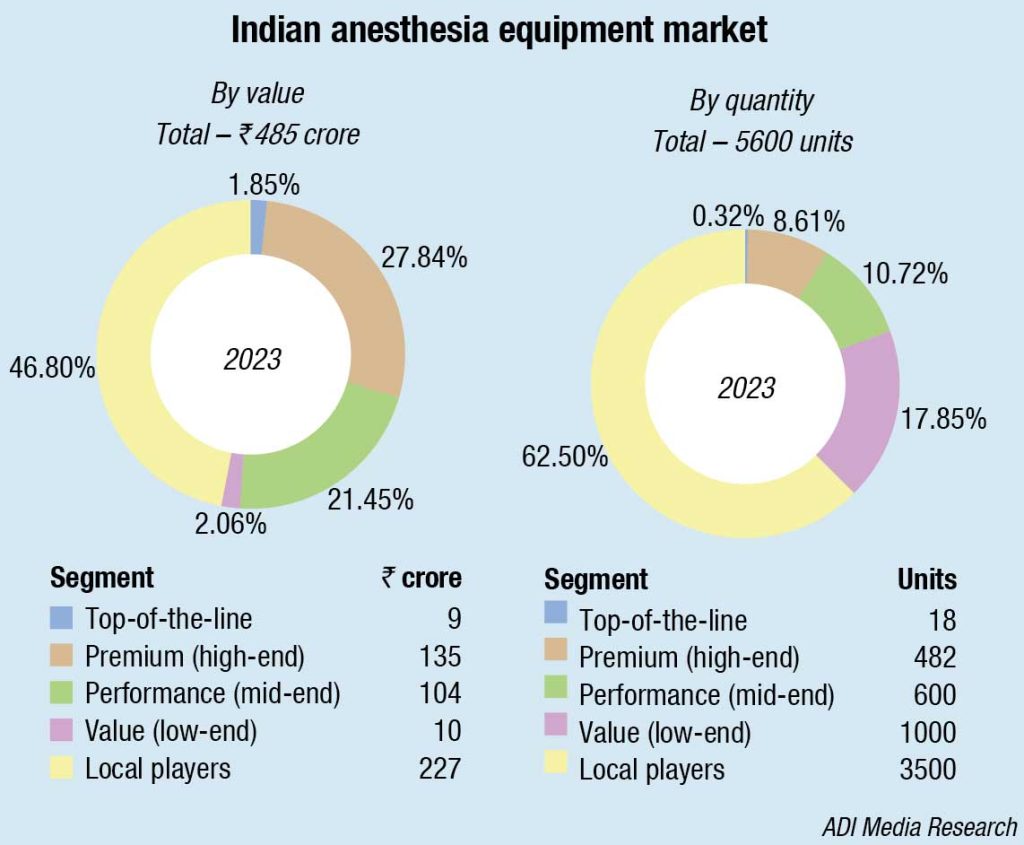
The premium, high-end machines continue to have 27-percent market share and, along with the performance segment that commands a 21 percent share by value, are procured by the discerning hospitals that need features as electronic vaporizers, fresh gas decouplers, digital gas mixers, and built-in AGMs (anesthesia gas monitors). The large numbers are sold in the value segment or by the local players in the unit price range of sub-₹120,000. Along with the established players, there are as many as 40 more brands that sell 5–10 machines each per annum.
|
Leading players-Indian anesthesia equipment market |
|
| Tier 1 | Draeger, Mindray, GE and BPL |
| Tier 2 | Allied Medical & Skanray |
| Others | Medec, Lowenstein, Maquet, Comen, Aeon and many others with sales of 5-10 machines each |
|
*Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian anesthesia equipment market. ADI Media Research |
|
Procurement by the hospitals in the Center and the BJP-run states has declined, partly to be attributed to the clause restricting imports from a country that shares land border with India added in the tender document, and also on the emphasis to restrict to Made in India machines.
Every manufacturer is moving toward providing advanced anesthesia devices that are not just tools; they are enablers of a patient-centric approach, ensuring that every breath matters. Combined with patient monitoring solutions, the anesthesia devices bring patient-relevant data to the point-of-care and ICU-quality ventilation therapy to the OR, such as lung-protective ventilation and minimal- and low-flow anesthesia.
Global market scenario
The global anesthesia machine market was valued at USD 8.84 billion in 2023, and is expected to grow at a CAGR of 9.21 percent over the next five years.
The market has witnessed rapid technological development and advancements in recent times, which is primarily driven by the rapid increase in minimally invasive surgeries, and increasing healthcare expenditure.
Recent advancements in local anesthesia delivery devices leverage concepts like the gate control hypothesis, using vibration to minimize pain during needle procedures. These innovations aim to improve patient comfort and contribute to the evolving landscape of anesthetic equipment.
VibraJect. Recently, a vibrating dental local anesthetic attachment was unveiled. It sends a strong enough high-frequency vibration to the needle for the patient to sense. On the basis of the gate-control theory, interference stimulation, can reduce pain.
DentalVibe. A recently developed device called DentalVibe vibrates during the administration of dental injections to stimulate the mechanoreceptors and lessen pain. The tool delivers percussive micro-oscillations to the injection administration site through a U-shaped vibrating tip that is handheld and cordless.
Accupal. It is a cordless device utilizing vibration and pressure to condition the oral mucosa during injections. It applies pressure and vibrates 360 degrees around the injection site, closing the pain gate to reduce discomfort. Accupal’s innovative approach enhances patient experience by minimizing pain and discomfort during the administration of injections.
Buzzy system. This instrument shaped like a bee, uses detachable ice wings and body vibration to obstruct pain-receptive fibers, reducing discomfort during local anesthesia administration. It employs both vibration and continuous cold near the injection site. Specifically designed to alleviate pain and anxiety in children during dental procedures.
By type, the workstation segment generated the highest revenue share in the market. Anesthetic workstations are equipped with various tools, such as anesthetic machines, physiological monitoring, and add-ons like active suction equipment and supplementary bag-valve-mask devices. In addition to administering volatile anesthetics, they also offer breathing and oxygenation. The workstations are favored by medical experts around the world for surgical procedures because of their versatility. Other segments are anesthesia delivery machines, anesthesia ventilators, anesthesia monitors, and other devices.
Within the anesthesia disposables segment, the anesthesia circuits segment registered the maximum revenue share in the market last year. The demand for anesthetic circuits is rising because of the frequency of respiratory ailments, including pulmonary embolism, chronic obstructive pulmonary disease, sleep disorders like obstructive sleep apnea, and increased surgeries. Governments and commercial organizations are expected to enhance their healthcare sector spending, stimulating market expansion. Other segments are anesthesia masks, endotracheal tubes (ETTS), laryngeal mask airways (LMAS), and other accessories.
Currently, the orthopedic segment has the largest revenue share in the market. This is a result of an increase in cases of bone- or muscle-related issues, a growing geriatric population, growing public awareness of muscular medical procedures, and ongoing developments that are enabling an expansion in the use of muscular medical procedures, all of which will aid in promoting the development of anesthesia devices. Other segments are neurology, cardiology, respiratory care, urology, general surgery, dental, and ophthalmology. Urology is expected to capture approximately 1/5th share of the market by 2030. There are pathology laboratories affiliated with medical care centers. Hospitals, ASCs, and clinics offer urological diagnostic and therapeutic services, and have significant infrastructure to perform invasive and non-invasive treatments that may not be available otherwise.
In December 2023, the World Health Organization (WHO) released data indicating that cancer is the leading cause of mortality, responsible for an estimated 10 million deaths in 2020. According to Cancer Research UK, approximately 27.5 million new cancer cases are projected to be registered in 2040, reflecting a 61.7-percent increase compared to 2018. Consequently, factors, such as the rise in chronic diseases, including cancer, are leading to an increased demand for surgeries, thereby fueling the growth of the anesthesia machine industry. Additionally, the growing demand for cosmetic procedures is a significant factor contributing to the rise in revenue in the anesthesia machine market.
The market faces a significant hurdle in the form of the expensive nature of anesthesia machines, particularly in regions with limited healthcare budgets and resource constraints. Furthermore, the lack of proficient professionals to operate anesthesia machines, particularly in regions with limited access to specialized training programs and healthcare professionals, is a key factor impeding market growth.
Another notable restraint is the compliance with stringent regulatory standards and approvals, which can pose challenges for manufacturers and limit market entry barriers for new players. Additionally, anesthesia machines require regular maintenance and servicing to ensure their proper functioning and compliance with safety standards, which can pose logistical challenges for healthcare facilities.
Regional insights. North America accounts for the major anesthesia machine market. The reasons are many, the most important being the rising number of hospitals and increasing healthcare expenditure, the significant growth in patient volume and the demand for healthcare services holding the largest chunk of the market share.
The European market is anticipated to exhibit the second-largest market share. This growth can be attributed to the widespread usage of modern medical care technologies and machines, such as anesthetic machines.
The Asia-Pacific market is expected to expand at a significant growth rate, driven by the rising healthcare awareness, increasing disposable income and rapidly growing population in this region.
The key players operating in global anesthesia machine market are Medtronic, GE HealthCare, Philips, Draeger, Getinge, Penlon, Heyer Medical, Aeonmed, Smith Medical, Spacelabs Healthcare, Covidien, Oricare, and Dameca A/S.
There is high competition among leading players. Numerous national and international vendors make the market competitive. Leading suppliers offer a broad spectrum of products, who also have the requisite technical, financial, and marketing resources, a large geographic footprint, and substantial R&D expenditures. Small- and medium-sized suppliers, on the other hand, have constrained financial and technical resources in addition to constrained product offerings. As a result, these providers cannot compete with well-known vendors regarding quality, dependability, and R&D. These factors will, therefore, continue to limit market growth.
The major strategies followed are partnerships as the key developmental strategy to keep pace with the changing demands of end users. For instance, in March, 2023, GE HealthCare came into collaboration with LeQuest to make digital simulation training for GE HealthCare’s anesthesia and respiratory devices. In June, 2021, Philips had signed an agreement with Elekta to advance complete and customized cancer care via precision oncology solutions.
Medtronic PLC is the major forerunner in the market. In October, 2022, Medtronic introduced the Neurovascular Co-Lab Platform, the platform designed for transforming ideas and technologies. This launch would propel collaboration and connections among physicians, start-ups, and institutions. GE HealthCare, SunMed, and Medline are some of the key innovators in the market.
Emerging trends and technological advancements in anesthesia
 Srishti Chauhan
Srishti Chauhan
Clinical Application Specialist, R&D,
Skanray Technologies Limited
The evolution of anesthesia technology has traversed distinct phases, each contributing to the refinement of patient care. The journey began with the advent of inhalation anesthesia, introducing agents like halothane and isoflurane. This marked a significant development, leading to the creation of anesthesia machines designed for precise administration of inhaled agents. Subsequently, the field progressed with advancements in monitoring, embracing technologies, such as pulse oximetry, capnography, and advanced blood pressure monitoring. These innovations markedly enhanced patient safety during anesthesia procedures, providing real-time insights into vital parameters.
Total intravenous anesthesia (TIVA) emerged as a pivotal phase, gaining popularity for its capability to allow precise control of drug delivery exclusively through intravenous means. This approach offered an alternative method for administering anesthesia with increased accuracy.
The article highlights the emergence of closed-loop anesthesia systems, representing a technological leap forward. These systems seamlessly integrate real-time patient data, automatic adjustments, and artificial intelligence (AI) to achieve personalized and adaptive anesthesia delivery. By overcoming dosing variations inherent in traditional methods, closed-loop systems significantly contribute to maintaining a stable anesthetic state while reducing adverse events.
The focus then shifts to technological advancements addressing lung protective ventilation and low flow anesthesia.
High-flow nasal cannula (HFNC) oxygen therapy takes the forefront, recognized for preventing hypoxemia during anesthesia, especially in surgeries with a heightened risk of prolonged apnea. HFNC delivers humidified and heated oxygen at high flow rates, catering to critical care scenarios.
Another notable advancement is the introduction of bellows-less ventilator technology, symbolizing a shift from traditional bellows-driven anesthesia machines to more advanced systems like piston-driven, volume reflector, and volume exchanger technologies. This transition aims to enhance precision in anesthesia delivery, providing more control over gas delivery.
The article underscores the commitment to low-flow anesthesia and lung protective ventilation, emphasizing safety, precision, and efficiency in anesthesia practices. Incorporating features like low-flow guidance software in anesthesia machines aligns with the ongoing efforts to advance patient care and surgical outcomes. In conclusion, the transformative impact of these innovations highlights a new era in anesthesia, promising improved healthcare efficiency and patient satisfaction.
Recent advances in technology
The realm of anesthetic technology is experiencing a seamless integration of progress, marked by ground-breaking innovations that transcend traditional boundaries. Recent advances have been made for local anesthesia, total intravenous anesthesia (TIVA), and the growing field of anesthetic nanomedicine, making modern anesthesiology highly dependent on technology.
Local anesthesia advancements, controlled-release formulations, and precision-guided injections are transforming conventional practices. This technological evolution aims to enhance the precision of local anesthesia administration, thereby minimizing side effects and optimizing patient comfort. As we move forward, a comprehensive overview emerges, synthesizing evidence from different studies and providing an overall understanding of the efficacy and safety of these localized innovations. The technological innovations collectively represent a significant step forward in improving the overall patient experience during dental procedures.
TIVA, a cornerstone of modern anesthesia practice, has contributed to the research and innovations related to TIVA conducted in the past ten years, leading to improvement in the field. The merits of TIVA were highlighted during Covid-19 pandemic, confirming its potential further in the post-Covid clinical practice as well, and advancement in digital technology with mobile apps has increased the scope of TIVA in day-to-day use. Here, technological strides, such as target-controlled infusion (TCI) systems and personalized anesthesia, based on patient characteristics, are redefining perioperative care.
Advancement in digital technology with mobile applications has increased the scope of TIVA in day-to-day use as a safe technique. Therefore, the advantages of TIVA, including improved control and a reduced incidence of adverse effects, come into focus. This application connects the dots between technological advancements and their role in shaping safer and more effective intravenous anesthesia.
Nanomedicine. The journey through the landscape of anesthetic technology continues by navigating the nanoscale innovations that are revolutionizing drug delivery in anesthesia. Anesthetic nanomedicines, operating at the forefront of nanotechnology, offer targeted and precise administration. The potential of nanomedicines to minimize side effects and contribute to personalized anesthesia emerges as a focal point. Despite some challenges associated with nanomedicine adoption, the transformative power of nanotechnology helps reshape the administration of anesthetic agents, leading to a reduction in medical errors and improved surgical outcomes, which will make new contributions to the development of anesthetics.
From local anesthesia’s precision to the advancements in intravenous administration and the promising applications of anesthetic nanomedicines, each aspect seamlessly connects to form a narrative of progress. The synergy of these interconnected advancements promises not only to redefine the landscape of anesthesia but also to elevate the standard of care.
As we traverse this integrated journey of innovation, the connection between these technological threads becomes evident. The exploration of localized pain management, the evolution of TIVA, and the applications of nanotechnology collectively contribute to a narrative that is greater than the sum of its parts. This seamless integration of progress stands as a testament to the collaborative efforts shaping the future of anesthetic technology, promising a more efficient, patient-centric, and technologically advanced landscape in the field of anesthesiology.
Technological developments in anesthetic equipment
CLADS. The landscape of an aesthetic equipment is evolving with rapid technological advancements, particularly in the realm of closed-loop anesthesia delivery systems (CLADS). Such systems are at the forefront of enhancing safety and efficacy in automated anesthesia delivery. The focus on safety is evident in the meticulous examination of the CLADS role in reducing risks, particularly in complex medical scenarios, such as cardiac surgery and for patients with heart conditions or those undergoing procedures at high altitudes.
In addition to addressing cardiac surgery challenges, CLADS extends its utility to environments with elevated altitudes. The unique physiological demands of high-altitude conditions require specialized considerations in anesthesia delivery. The closed-loop system is tailored to mitigate risks and enhance safety in these environments. This adaptation showcases the versatility of closed-loop systems in catering to diverse medical scenarios.
Furthermore, they shed light on the practical aspects of working with TIVA. The integration of technology, specifically introducing target-controlled infusion (TCI) and CLADS, enhances the precision and control of intravenous anesthesia. This technological synergy ensures a seamless and effective administration of anesthesia, aligning with the broader trend of leveraging advancements to refine the intricacies of anesthetic procedures.
Another advancement in anesthetic technology extends beyond closed-loop systems, encompassing the domain of high-flow nasal cannula (HFNC) oxygen therapy.
High-flow nasal cannula (HFNC) oxygen therapy is a commonly used respiratory intervention to support patients with acute respiratory failure. It has also demonstrated positive outcomes in chronic hypercapnic respiratory failure, particularly in stable chronic obstructive pulmonary disease (COPD) patients. Aerosol delivery through HFNC allows uninterrupted respiratory support, with vibrating mesh nebulizers showing promise for enhanced drug deposition.
Another application of HFNC technology can be seen by examining its application in both human and veterinary patients. This cross-disciplinary exploration signifies the versatility of HFNC beyond traditional medical boundaries. It has been proposed that high-flow nasal oxygen therapy (HFNOT) improves pulmonary mechanics and reduces respiratory fatigue via reduction of anatomical dead space, provision of low-level positive end-expiratory pressure (PEEP), provision of constant FiO2 at rates corresponding to patient requirements and through improved patient tolerance.
In parallel, HFNOT has demonstrated its ability to enhance patient outcomes in cases of hypoxemia, although most of the evidence stems from studies conducted in intensive care units. Within perioperative settings, ongoing research is shedding light, yet there remains a demand for supplementary evidence to establish its efficacy. HFNOT could play a pivotal role in enhancing preoxygenation and may also be valuable after extubation.
As these scientific researches unfold, a common thread emerges – the intersection of technological developments and their tangible impact on anesthetic equipment. The evolution of HFNC exemplifies the fusion of clinical insights, technological innovation, and a commitment to advancing respiratory support. The fluidity of this narrative reflects the interconnected nature of these technological developments, each thread weaving seamlessly into the fabric of anesthetic progress.
Furthermore, the convergence of HFNC with advancements in anesthesia technology amplifies the potential for synergistic solutions. The dynamic interplay between respiratory support mechanisms and broader technological trends underscore the integrated approach to patient care. From refining clinical practices in adult acute care to addressing specific needs in neonatal settings, HFNC stands as a testament to the continuous refinement of anesthetic equipment to meet evolving healthcare demands.
Transforming anesthesia – Revealing technological progress and emerging developments
 Aditya Kohli
Aditya Kohli
CFO & Director,
Allied Medical Limited
In the ever-evolving landscape of healthcare, technological advancements continue to reshape the field of anesthesia, enhancing patient safety, precision, and overall efficiency. Among the latest breakthroughs are electronic gas mixing with digital flowmeters, electronic hypoxia devices, and clinical decision support tools, notably fresh gas flow optimization. The traditional practice of manual gas mixing in anesthesia is being replaced by electronic gas mixing systems integrated with digital flowmeters. This innovation allows for precise control over the composition and flow rates of anesthetic gases, ensuring accurate administration tailored to individual patient needs. The result is improved anesthesia delivery, minimizing the risk of complications and enhancing patient outcomes. Electronic hypoxia devices mark another milestone in anesthesia technology. These devices closely monitor oxygen levels in real-t me and automatically adjust the flow to prevent hypoxia, a condition where the body is deprived of adequate oxygen supply. This automated response significantly reduces the likelihood of human error, offering an added layer of safety during surgical procedures. Fresh gas flow optimization has emerged as a critical component in the quest for more sustainable and cost-effective anesthesia practices. Clinical decision support tools analyze data in real time, providing anesthesiologists with recommendations for optimizing fresh gas flow rates, based on patient parameters. This not only ensures a more economical use of resources but also contributes to a greener, environmentally friendly approach by minimizing gas wastage. The integration of these technologies into anesthesia practice goes beyond mere efficiency; it is about elevating patient care to new heights. Precise gas control, automated hypoxia prevention, and intelligent decision support systems collectively contribute to safer and more tailored anesthesia delivery. Patients can benefit from reduced risks, quicker recovery times, and a more personalized healthcare experience. As we navigate the future of healthcare, the amalgamation of electronic gas mixing, hypoxia devices, and clinical decision support tools in anesthesia promise to redefine the standards of care. The synergy of these technological advancements not only streamlines processes but also exemplifies a commitment to patient safety, setting a new paradigm for the practice of anesthesia in the 21st century.
The development in anesthetic equipment emerges in the form of a portable wireless dental anesthesia delivery device. This technology enhances the accessibility and flexibility of anesthesia administration. The device represents a departure from traditional methods, offering a portable and efficient solution that aligns with the evolving needs of dental practitioners. This shift underscores the industry’s commitment to advancing technology to optimize patient care and procedural efficiency.
These technological developments not only shape the present landscape of anesthetic equipment but also pave the way for a future where precision, adaptability, and patient-centric care remain at the forefront of respiratory support strategies.
Artificial intelligence
AI has rapidly emerged as a transformative force in various domains of healthcare, and its impact on anesthesiology is no exception.
The ability of AI algorithms to analyze patient data, such as vital signs and medical history in real time enables anesthetic equipment to tailor the dosage and type of anesthesia to each patient’s unique characteristics, improving the overall safety and efficacy of the procedure.
Another application of AI in anesthesiology extends across the entire perioperative process, encompassing preoperative assessment, intraoperative monitoring, and postoperative care. The integration of AI algorithms demonstrates significant potential in improving patient care by enabling personalized risk assessments, optimizing drug delivery, and implementing advanced monitoring systems.
Furthermore, the incorporation of AI in anesthetic equipment goes beyond traditional monitoring methods. By continuously analyzing real-time data, AI algorithms can identify patterns and trends that may indicate potential issues before they escalate. This proactive approach allows anesthesiologists to intervene promptly, preventing adverse events and ensuring a higher standard of patient safety.
Automation not only streamlines processes but also reduces the cognitive load on anesthesiologists, allowing them to focus on critical decision making. From automated drug delivery systems to predictive modeling for patient responses, AI contributes to increased efficiency in the administration of anesthesia.
As the field of anesthesiology continues to embrace AI, the need for robust research and validation becomes evident. Rigorous testing and validation protocols ensure that AI applications in anesthetic equipment meet the highest standards of reliability and contribute positively to patient outcomes.
The integration of AI into anesthetic equipment has undoubtedly ushered in a new era of precision, efficiency, and safety in anesthesiology.
Collaborative efforts among healthcare professionals, technology developers, and policymakers will be crucial as healthcare systems evolve to accommodate these advancements, ensuring the responsible integration of AI and unlocking its full potential in shaping the future of anesthesia.
However addressing challenges related to data security, interpretability, and the evolving dynamics of the patient-doctor relationship is essential. The implications for patient care are profound, with the potential for improved outcomes, reduced complications, and heightened overall satisfaction.
Within this landscape of innovation and progress, challenges persist. The delicate balance between embracing technological advancements and addressing economic considerations is a notable hurdle. The intersection of industry players, including private anesthesia groups, hospital systems, and private equity firms, sometimes necessitates strategic decision making. The quest for optimal patient care must co-exist with financial viability and operational efficiency, creating a complex dynamic that requires careful navigation.
As the industry embraces technological advancements, a broader perspective on anesthesia technology trends comes into focus. The evolution of anesthesia technology encompasses diverse facets, from equipment design to monitoring systems and procedural techniques. This comprehensive approach is essential in addressing the multifaceted challenges faced by anesthesia professionals. The trends in anesthesia technology underscore the industry’s commitment to staying abreast of advancements that enhance patient safety, streamline workflows, and contribute to overall procedural success.
In the dynamic landscape of anesthetic advancements in coming years, the fusion of cutting-edge technologies and evolving practices emerges as a beacon for the future. From the transformative impact of AI on precision anesthesia to the strategic challenges faced by the industry players, the narrative unfolds with a commitment to innovation and patient-centric care. This interconnected journey signifies a paradigm shift, where seamless integration of AI, technological developments, and industry perspectives converge to redefine the standards of anesthesiology.
As we move forward, the promise of enhanced efficiency, safety, and patient outcomes stands as a testament to the collaborative efforts shaping the future of anesthetic technology.
Second Opinion:-
Features and technological advancements impact decision making hugely.