Trends
How flexible ultrasound stickers can detect post-surgery complications
Researchers at Northwestern University and Washington University School of Medicine in St. Louis found a new way to use ultrasound to monitor patient health.
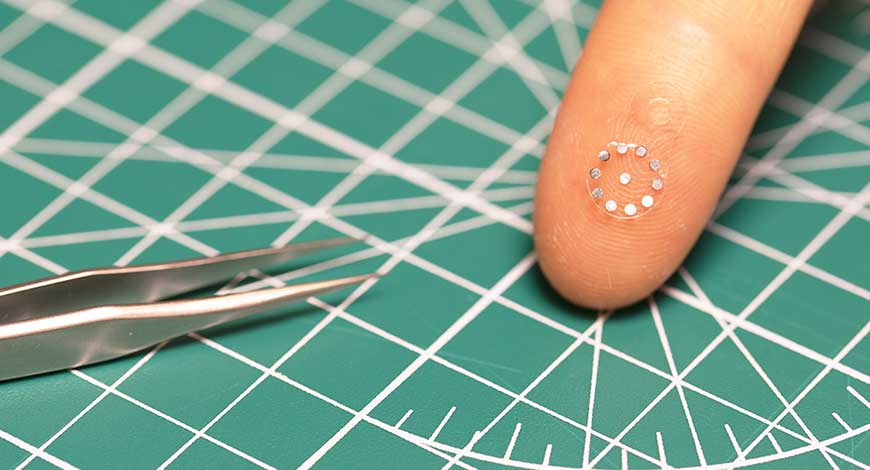
This first-of-its-kind sticker enables the monitoring of organs and deep tissues through a simple ultrasound device. When attached to an organ, the soft, tiny sticker changes in shape in response to the body’s changing pH levels. This can serve as an early warning sign for post-surgery complications, like anastomotic leaks. Clinicians can view the shape changes in real-time through ultrasound imaging.
According to the researchers, no existing methods can reliably and non-invasively detect anastomotic leaks. The sticker they developed can enable earlier interventions than previously possible. Then, when the patient fully recovers, the biocompatible, bioresorbable sticker dissolves, eliminating the need for surgical extraction.
The team published data from a study evaluating three different types of stickers made from hydrogel materials. Published in Science, the study spanned small and large animal models, looking at anastomotic leaks from the stomach, small intestine and pancreas.
“These leaks can arise from subtle perforations in the tissue, often as imperceptible gaps between two sides of a surgical incision,” said Northwestern Engineering’s John A. Rogers, who led device development with postdoctoral fellow Jiaqi Liu. “These types of defects cannot be seen directly with ultrasound imaging tools. They also escape detection by even the most sophisticated CT and MRI scans. We developed an engineering approach and a set of advanced materials to address this unmet need in patient monitoring. The technology has the potential to eliminate risks, reduce costs and expand accessibility to rapid, non-invasive assessments for improved patient outcomes.”
Chet Hammill, who led the clinical evaluation and animal model studies at Washington University with collaborator Matthew MacEwan, an assistant professor of neurosurgery, sought out Rogers to produce improved outcomes for patients with anastomotic leaks. Rogers’ team previously developed bioresorbable electronic devices to serve as temporary implants.
“We like to monitor patients for complications for about 30 days,” Hammill said. “Having a device that lasts a month and then disappears sounded ideal.”
Improving ultrasound
Rogers surmised that the team could enhance current imaging methods rather than develop new imaging systems for this technology. Ultrasound represented an inexpensive, available option that didn’t require large, cumbersome equipment or expose patients to radiation or other risks.
The team noted that ultrasound fails to reliably differentiate between bodily fluids, like blood and gastric fluid, for example.
“The acoustic properties of the leaking fluids are very similar to those of naturally occurring biofluids and surrounding tissues,” Rogers said. “The clinical need, however, demands chemical specificity, beyond the scope of fundamental mechanisms that create contrast in ultrasound images.”
The team’s approach to address this issue utilized tiny sensor devices that are readable by ultrasound. They made their small, tissue-adhesive sticker from a flexible, chemically responsive, soft hydrogel material. Then, they embedded small, paper-thin metal disks into the layers of the hydrogel. When the sticker encounters leaked fluids, it swells.
Visualizing the sticker
When the sticker swells, the metal disks within it move apart in a way that ultrasound can see.
“Because the acoustic properties of the metal disks are much different than those of the surrounding tissue, they provide very strong contrast in ultrasound images,” Rogers said. “In this way, we can essentially ‘tag’ an organ for monitoring.” Because the need for monitoring extends only during a postsurgical recovery, Rogers team designed these stickers with bioresorbable materials. They simply disappear naturally and harmlessly in the body after they are no longer needed.
Computational collaborator Yonggang Huang, the Jan and Marcia Achenbach Professorship in Mechanical Engineering and professor of civil and environmental engineering at McCormick, used acoustic and mechanical simulation techniques. These helped to guide optimized choices in materials and device layouts to ensure high visibility in ultrasound images. This applied to stickers located at deep positions within the body as well.
“CT and MRI scans just take a picture,” Hammill said. “The fluid might show up in a CT image, but there’s always fluid collections after surgery. We don’t know if it’s actually a leak or normal abdominal fluid. The information that we get from the new patch is much, much more valuable. If we can see that the pH is altered, then we know that something isn’t right.”
The team created stickers across a range of sizes, with the largest coming in at 12 mm in diameter and the smallest just 4 mm in diameter. The metal disks within them register at just 1 mm in diameter.
Rogers says the small size of the disks means radiologists could have difficulty assessing the images manually. So, the team developed a software that can automatically analyze the images, detecting disk movement with high accuracy.
Testing the sticker
To evaluate the stickers, Hammill’s team conducted the animal model testing. In the studies, ultrasound imaging consistently detected changes in the shape-shifting sticker, even as deep as 10 cm in the tissues. When exposed to fluids with abnormally high or low pH levels, the sticker’s shape changed within minutes.
According to Rogers and Hammill, the researchers feel the device could be implanted after a surgical procedure. Additionally, they envision delivery through a syringe thanks to the small size and flexibility of the sticker.
“These tags are so small and thin and soft that surgeons can easily place collections of them at different locations,” Rogers said. “For example, if an incision extends by a few centimeters in length, an array of these tags can be placed along the length of the site to develop a map of pH for precisely locating the position of the leak.”
The team believes that next steps could include similar tags that could detect internal bleeding or temperature changes.
“Detecting changes in pH is a good starting point,” Rogers said. “But this platform can extend to other types of applications by use of hydrogels that respond to other changes in local chemistry, or to temperature, or other properties of clinical relevance.” Medical Design & Outsourcing














