Buyers Speak
Nine months into COVID and lockdown – What do we do now?

At the time of writing this article, a new strain of coronavirus has been identified, which is believed to be 70 percent more infectious than the original virus. Flights have been cancelled to and from UK and a new sort of stringent than ever lockdown imposed in parts of UK. While the vaccine itself is claimed to be effective on this new strain, residual concerns on vaccine remain with isolated reports of bell’s palsy as a side effect coming in. Closer to the home, the Serum Institute has been asked for more data on the vaccine’s immunogenicity. And the single isolated alleged case of neurological and psychological side effect continues to remind us of the importance of a strong and robust vaccine approval mechanism. All this and more, makes one to believe that the virus is going to be with us for some more time and it will be a good time before the things go back to normal.
So, what do we do? Do we wait and hope for the crisis to end on its own? Or do we simply learn to live with it and hope that something similar never recurs? I argue that while the scientific community is doing their best to come up with vaccine, we prepare ourselves to change the neglected system for the best to happen. This includes addressing the long systematic challenges we have been seeing in the system and where we have the maximum traction in terms of political and social will. And how do we do it?
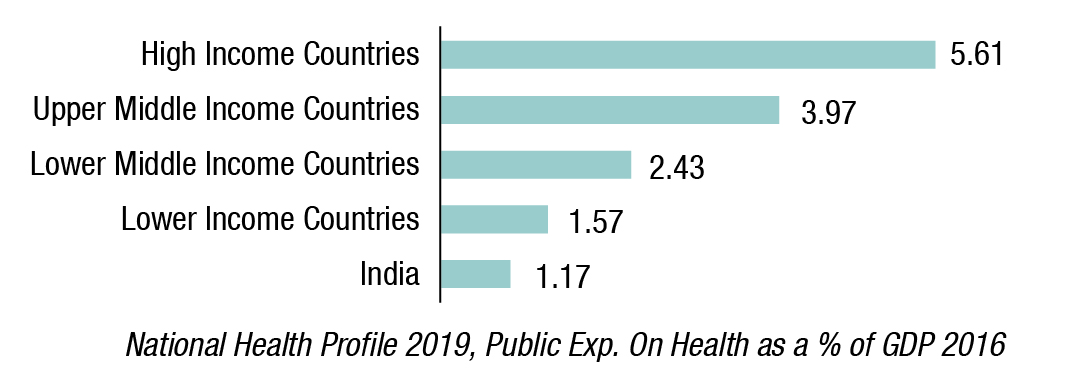
Increase the public health spend
Multiple evidences have flown in citing that a decent public healthcare spend has a cross multiplier effect not only in terms of healthcare gains, but also gains in GDP production, labor markets, Insurance Markets and even in as something basic as child education. This public spend is also believed to be a better way of targeting the poor population which is predisposed in terms of catastrophic expenditure. Alas, in India, the public health spend is a meagre amount as compared to other countries. (National Health Profile 2019, Public Exp. On Health as a % of GDP 2016). While different reports, including the 15th Finance Commission has said, this will happen, we will get to know it only when budget is announced.
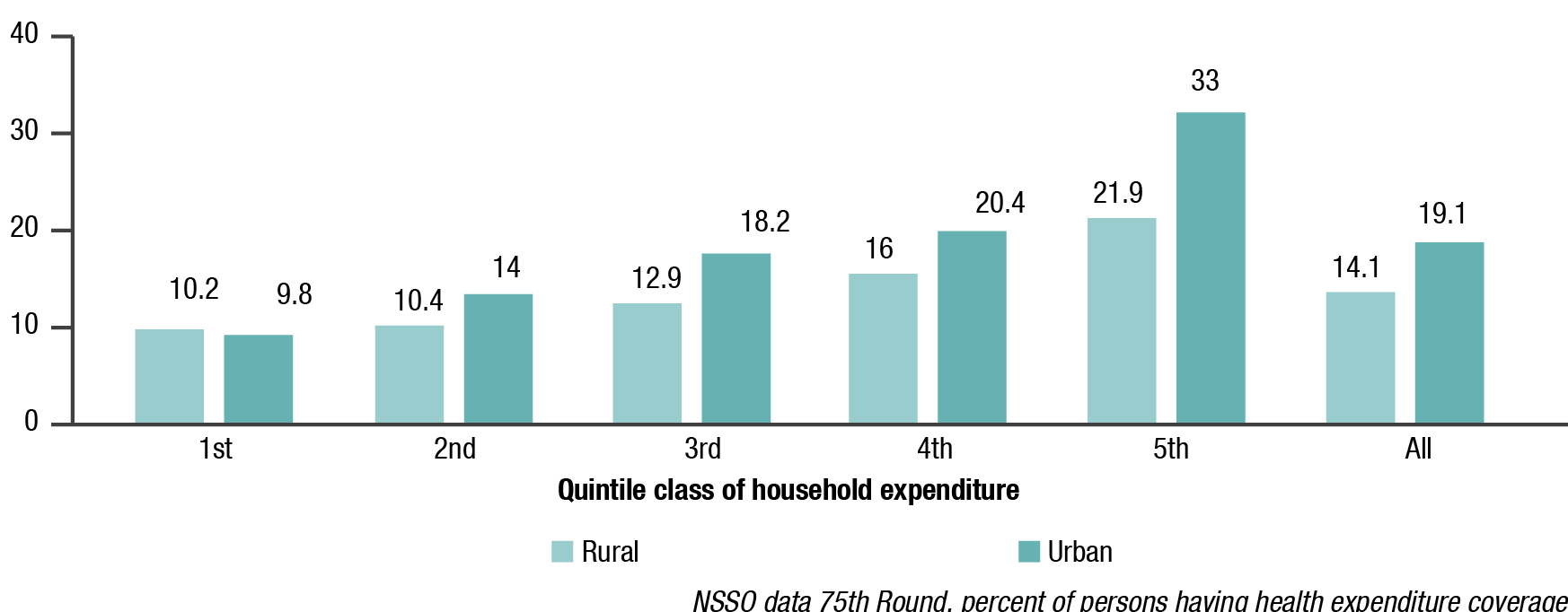
Bring in the insurance reforms and make healthcare insurance available to all
While the PMJAY has a massive potential of catering to 500 million people, data shows that only ~125 million odd health cards have been issued. Further, the people who have access to other forms of insurance, actual support happening is rather limited (NSSO data 75th Round, percent of persons having health expenditure coverage), especially for the bottom income quintile making them highly predisposed to health shocks and poverty. Reforms have been announced for including Missing Middle population (hitherto uncovered population) in some form of contributory, yet subsidized insurance scheme, but the same needs to be accelerated and rolled out.
Expedite the National Digital Health Mission
Much has already been emphasized on the importance of electronic medical and personal health records, and the importance of making them universal, consistent across different stakeholders and using them for public health policy making. A successful roll out of NDHM requires an aspirational buildup of capacities especially in things like making registries and providing unique IDs. It also requires a much more understanding of data protection laws and the pending Personal Data Protection Bill. This is a unique and much aspirational initiative launched and should be expedited in all earnest.
Develop public private partnerships
The present crisis highlighted how woefully inadequate we are in terms of engaging private sector in healthcare delivery. Despite having the capacities, the majority of diagnostic tests continued to happen in public sector for one reason or others. Charges and counter charges continued to fly of private hospitals not admitting patients, overcharging, and relying on non-evidence-based treatment strategies. Courts had to intervene, and rules were made under Disaster Management Act. If anything, this has only widened the trust deficit between the two sectors. Lessons learnt, we should now focus our energies on engaging the two sectors better, identify respective strengths and address genuine concerns.
Train human resource and plug in vacancies
With ~0.7 doctors/1000 population and ~1.8 nurses/midwives per 1000 population, we are sadly inadequate in terms of manpower. The corresponding prescribed norms are 1 and 4 to be minimum. The situation is even wary in terms of specialists and super specialists in India.
While the National Medical Commission promises to be an advancement over MCI, in the sense that it focuses on improving output rather than input infrastructure requirements, standardizing and streamlining the medical education and post-graduation, much remains to be seen on how it is rolled out on ground and how the states adopt it. Further, the recent concerns on integrating AYUSH courses with Allopathic courses needs to be adequately handled with any concerns being addressed in a consensus-based manner.
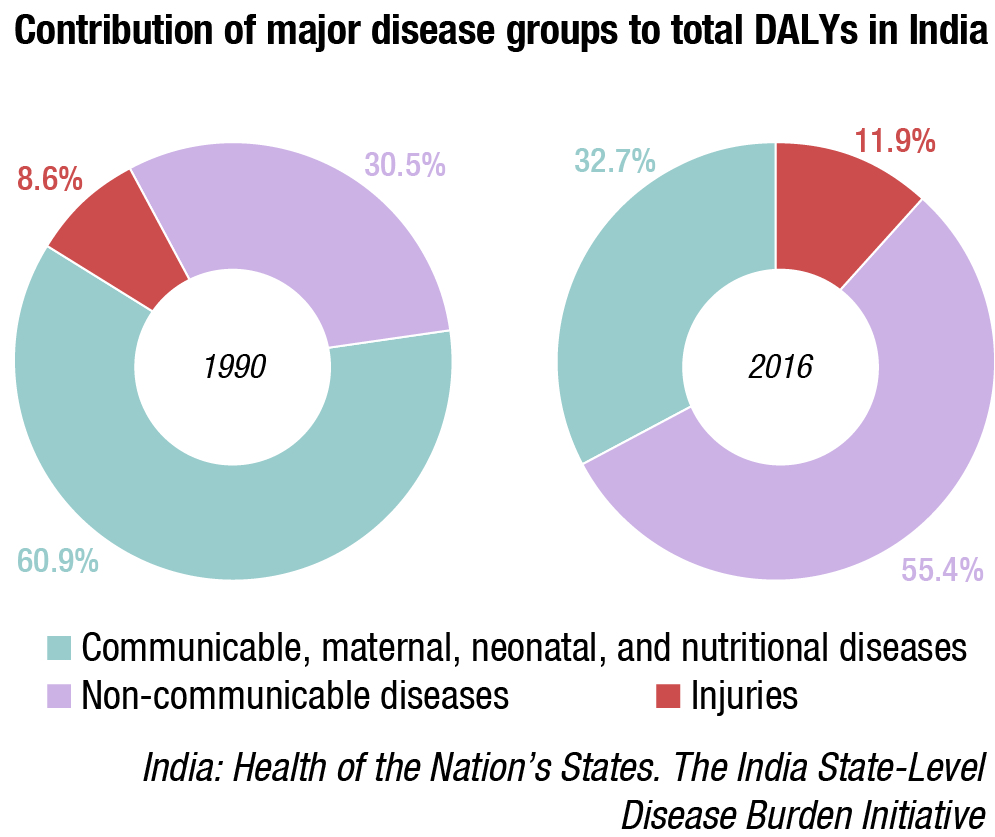
Curb hyperbolic tendencies and develop a healthy lifestyle behavior
No measure of healthcare reforms is going to be enough if we continue to lead an unhealthy lifestyle. We are already witnessing a high disease burden from non-communicable disorders which are to a certain extent linked to lifestyle behavior India: Health of the Nation’s States. The India State-Level Disease Burden Initiative. The steps on Electronic Nicotine Delivery devices is welcome. But much more needs to be done to ingrain a culture of leading a healthy lifestyle in our way of living.
Identifying this above to–do list is probably the easiest task in the entire array of reforms that the country might require, as we wait for an end solution to COVID-19 crisis. However, this list is by no means comprehensive and not an easy task to execute upon. Multiple socio-economic-demographic-political-cultural challenges need to be worked upon to push these on the ground. With health being a state subject and with different states being at different trajectories of healthcare maturity, even the basic proper institutional and governance framework needs to be defined.
Further, in an era of decreasing revenues and increasing deficits, the source of money needs to be identified, and allocation defined among competing claims and priorities. But that should not deter us from focusing and advancing on what seems immediately feasible and warrants most attention. Handling this basic human necessity might be the most fulfilling part of never let a crisis go waste dictum.














