Buyers Speak
Universal health coverage in Asian perspective

Universal health coverage (UHC) is a state-sponsored health policy, which will ensure that all people get quality health services they deserve, without experiencing financial hardship. UHC is a pivotal element to achieving progress on the sustainable development and growth for any economy. Generally, UHC has two magnitudes – Access to common mass, where accessing quality healthcare is a challenge, and the other dimension is financial protection. The regional average for the UHC essential health services index is 64 percent in 2022, compared with 46 percent in 2010. On the other hand, over 65 million people are pushed into poverty because of out-of-pocket health expenditure.
Universal health coverage is an ecosystem sponsored by the state that all people obtain the health services they need without risking financial hardship from unaffordable out-of-pocket payments. On the contrary, health insurance is operated by the public and private organizations, where the quantum and extent of medical expenses is covered in accordance with the amount of premium paid.
Benefits of UHC
- A state-sponsored health policy, which will ensure that all people get quality health services they deserve.
- General public will not experience financial hardship from unaffordable out-of-pocket payments.
- It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care.
Thailand is among the few countries in the Southeast Asia region, or among middle income countries worldwide, that boasts of a UHC system, which allows access to publicly-funded healthcare without any co-payments and covers 98 percent of the population. UHC costs are financed through general taxation. The UHC scheme is managed by the National Health Security Office and implemented by the Ministry of Public Health through a network of 953 hospitals and 9765 health centers, reaching all sub-districts in the country. As UHC was initiated in Thailand in the timeline 2001 to 2011, life expectancy at birth rose from 71.8 to 74.2 years. There has been a significant decline in infant deaths from 100 per 1000 live births before 1970 to 9.5 per 1000 live births in 2017. Cost sharing is minimal, or almost nil, in Thailand’s UHC model. Following the implementation of UHC, previously massive health impoverishment has been significantly reduced; and healthcare has improved significantly and with more equity.
Today UHC covers the entire Thai population of 66.3 million persons. The Thai government’s attempt to merge all the schemes initially met with stiff resistance from beneficiaries. A unified national health insurance scheme was launched, accumulating all three existing schemes – (i) the civil servants’ scheme, covering 5.7 million people; (ii) the social security scheme under the labor ministry, covering 12.3 million people; and (iii) the universal coverage scheme under the public health ministry, covering 47.8 million people or 72 percent of the population.
Healthcare in Japan is, generally speaking, provided free for Japanese citizens, expatriates, and foreigners. Medical treatment in Japan is provided through UHC. This system is available to all citizens, as well as non-Japanese citizens staying in Japan for more than a year. One must enroll through their employer and their insurance contributions will be deducted automatically from their salary; if not, they must remember to pay the NHI tax regularly. Self-employed and unemployed people must enroll in the National Health Insurance plan at their local government office. Their NHI tax is determined based on income. The healthcare system in Japan provides free screening processes for certain diseases, infectious disease control, and prenatal care. Under the healthcare system in Japan, the patient accepts responsibility for 30 percent of the medical costs, and the government pays the remaining 70 percent.
Almost all South Koreans (97 percent) are covered by the National Health Insurance Service (NHIS) and pay NHIS premiums according to their income levels or property values. The other 3 percent, who are medical aid (MA) recipients, are unable to pay premiums, and their medical costs are covered by the government. Both NHIS and MA cover healthcare expenditures (outpatient, inpatient, diagnostic testing fees, and prescribed drugs) for an out-of-pocket cost, ranging from 0 to 20 percent; however, due to the pandemic, the South Korean government terminated all out-of-pocket costs associated with Covid-19-related health services.
Taiwan adopted a national health insurance system in 1995. It is a government-administered insurance-based national healthcare system. Taiwan has a single payer system for healthcare. The characteristics of the Taiwanese system include good accessibility, comprehensive population coverage, short waiting times, relatively low costs, and a national health insurance databank for planning, monitoring, and evaluating health services. The revenue for the NHI program comes from several sources – employees, employers, and the government, both national and local. There are special programs for different degrees of governmental premium subsidies for-low income populations and disadvantaged populations.
BPJS was formed in accordance with the SJSN Indonesia law, which was embodied in the Indonesian law number 24 of 2011 concerning the social security administering body (BPJS) to manage social insurance in Indonesia. Almost all Indonesians have become BPJS health participants. This amount is something to be grateful for and appreciated. The number of BPJS health participants reached 220.6 million people or about 83 percent of Indonesia’s population of 264 million.
Ayushman Bharat (PMJAY) was launched in India as a step toward universal health coverage (UHC). The concept covers three key elements – access, quality, and financial protection. India is committed to achieving UHC for all by 2030, which now has achieved sustainable development goals of 3.8. There were similar initiatives from various state governments. All the districts of West Bengal are covered under the Swasthya Sathi scheme and 45 lakh families, covering nearly 2.5 crore population, are benefitted by the scheme. Similarly Karnakata government has rolled out Arogya Bhagya, where 1.4 crore households will get cashless treatment up to Rs 1.5 lac in government and private hospitals. All these schemes cover a vast volume of population. Because of the prevailing low rates and prices, implementing such schemes is quite difficult in private hospitals.
Since it emerged from its years of isolation, Myanmar has scaled up its efforts to achieve UHC. The government adopted the National Health Plan (NHP) (2017 to 2021) to strengthen the healthcare system and set out a path toward achieving UHC. The aim of the NHP is to extend access to a basic essential package of health services (EPHS) to the entire population while gradually increasing financial protection. There are several challenges facing the healthcare system. Most important is chronic underfunding of the healthcare sector. Public spending on health has been persistently low over the last 20 years, teetering around 1 percent of GDP.
The health system of Bangladesh is experiencing a double burden of diseases, low service coverage, and a lack of effective financial-risk protection mechanism. Bangladesh has a pluralistic healthcare system, which is highly unregulated. In Bangladesh, less than 1 percent population has any form of health-coverage scheme. Approximately 3.8 percent of total population or 0.6 million people are pushed to poverty because of the out-of-pocket expenditure.
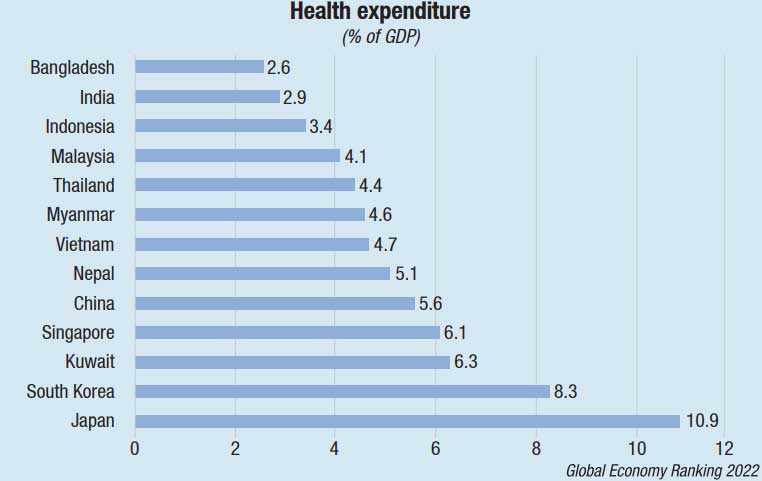
In Asia, 95 percent health coverage has been achieved in China, Japan, Singapore, Thailand, and South Korea. India and Indonesia began implementation of a UHC program, aiming to achieve UHC within the next few years. There are variations in service coverage that exist across the Asian countries; for example, Thailand covers prescription medications whereas benefits packages in China are limited to inpatient services with reimbursement for select chronic diseases. The out-of-pocket expenditure across the region varied from 11.3 percent in Thailand to 56.8 percent in Singapore. Bangladesh and Myanmar are severely lagging behind. The main challenge in Asia is to overcome regional variations whereas UHC implementation in Thailand can be an effective model.
Approximately 95 percent of Korea’s population is insured mostly financed through the National Health Insurance (NHI) system and generally delivered by private health providers. Taiwan relied on incentives, public and private partnership and effective regulations to create an effective UHC ecosystem. Taiwan’s experience holds a valuable lesson for other nations. India is committed to accomplish the UHC by 2030. The Central and State government should encourage public and private partnership and involve the private players in price discussion. This will ensure UHC success story in India.














