Anesthesia Equipment
Anesthesiology At The Cutting Edge

Technological advances have helped improve safety and quality of anesthesia, and are paving the way to semi-autonomous or even possibly completely autonomous surgery and delivery of anesthesia.
During the last decades, the risks associated with anesthetic care have dramatically reduced. Technological advancement and automation have played a significant role in improving patient safety, as well as the working environment of anesthesiologists. Anesthesia Information and Management Systems (AIMS) with integrated decision support, target-controlled infusion systems, better design of anesthesia machines, closed-loop delivery of anesthesia, and point-of-care ultrasound guided procedures, are some examples.
The trend for technological innovations continues. Robots have been developed to establish peripheral and central venous access, to perform endotracheal intubations, and to assist the administration of regional anesthesia. Tele-anesthesia offers the possibility of distant preoperative assessment of the patient’s fitness for anesthesia, aid of trained personnel to perform anesthetic tasks, and the control of anesthesia delivery in a distant location with the use of automated anesthesia drug delivery systems to maintain a target depth of anesthesia.
The new millennium has witnessed exponential progress and developments in technology occurring at an unprecedented scale. This, on one hand, is contributing toward improvement in provision of healthcare, yet on the other, is changing the face of medicine itself. There is a paradigm shift in medicine unfolding, which is likely to render anesthesiologists specialty irrelevant unless they align it with the needs of the future.
There are two main drivers for this change, namely, the future demographics and the global healthcare bill. The United Nations has estimated that by 2050, a fifth of the global population will be comprised of those aged above 65 years. This is likely to see a rise in a myriad of age related chronic health problems. The global healthcare spending is projected to expand from the current level of around USD 8 trillion to USD 18.28 trillion by 2040. Experts are trying to explore and devise ways and means to curtail this expense to more affordable levels. This has led them to revisit the way anesthesiologists see the divide between health and disease.
Indian market dynamics
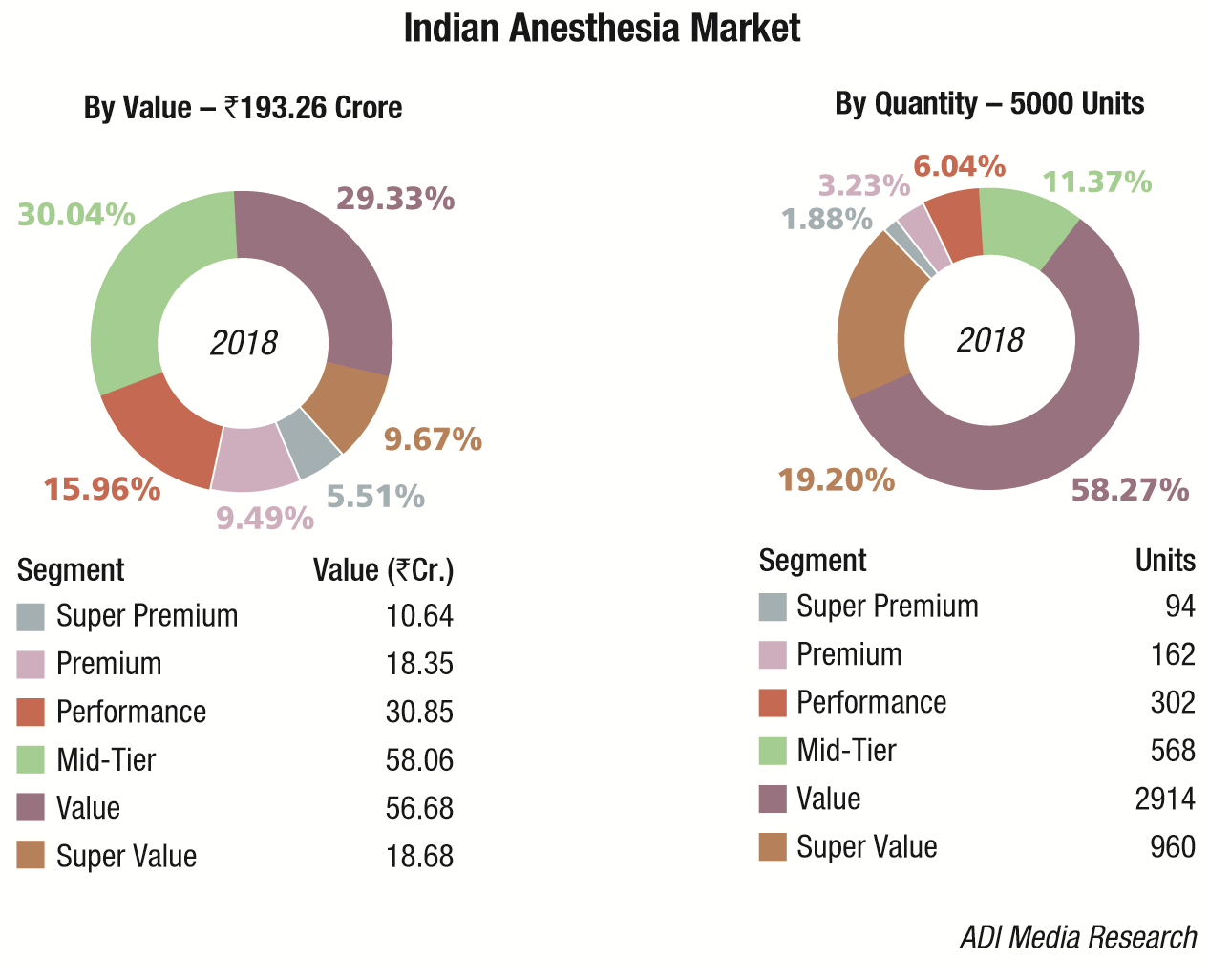
The Indian anesthesia equipment market in 2018 is estimated at Rs 193.26 crore, at 5000 units.
There are a handful of players in this segment who import the systems every quarter. These include Drager, Mindray, Spacelabs, BPL, Meditech, and Skanray,, with GE dominating the segment at an approximate 40 percent market share. Mindray had a very good year and found major success in the tenders invited by the government, having ensured that it was present in every price bucket. It may be safely assumed that the indigenous sector contributes 14 percent to this market.
| Major Vendors in Indian Anesthesia Equipment Market – 2018* | |||
|---|---|---|---|
| Tier I | Tier II | Tier III | Tier IV |
| GE | Drager | Mindray | Spacelabs, BPL, Meditech, Skanray, Allied Medical, local and regional brands |
| *Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian anesthesia equipment market. | |||
| ADI Media Research | |||
This is a price driven market with the government continuing to buy premium products, and the smaller nursing homes and medical facilities in tier-II and tier-III cities procuring the super value and value range of products. The emphasis continues to be on quality at affordable cost, and reliable after sales service.
Advancements in digital technology are driving a new generation of smart techniques in the anesthesia domain. Device manufacturers are focusing on exploring opportunities to improve the efficiency of anesthetic gas delivery to address the cumulative requirements of extra flexibility, increased patient safety, and improved patient care.
Global market
Global anesthesia equipment market is projected to witness a CAGR of 8.27 percent to reach the total market size of USD 13.3 billion by 2023, increasing from USD 8.9 billion in 2018, estimates ResearchAndMarkets. The vast increase in the number of surgical procedures undertaken across the globe every year has played a major role in the growth of the anesthesia equipment market. The most rapid increase was observed for laparoscopic hysterectomies. As every surgical procedure can be painful, anesthesia is administered to the patient during surgical procedures to keep patients pain free and unconscious during the procedure. Technological advancements, owing to increasing investments by major players in research and development, are enhancing the efficiency and reliability of these machines. Advanced anesthesia machines come with advanced ventilators, graphical displays, and other features integrated to ensure the safest possible experience for the patients which is increasing their adoption among the end-users, thereby augmenting the market growth. In addition, large patient pool and increased disposable income in emerging markets are expected to further boost the market in coming years.
North America and Europe are considered as key regional markets owing to presence of advanced medical facilities. Higher healthcare expenses capacity and shifting preference of patients toward home care over hospital care in these regions are boosting product demand. In addition, favorable government policies in these regions are also anticipated to propel the market growth in these regions in the years to come.
The Asia-Pacific region is also expected to have significant growth over the next few years. This growth can be credited to the rising healthcare awareness and consumer disposable income levels. India and China, in particular, are more promising economies in the Asia-Pacific region due to increasing number of hospitals as a result of the presence of target population base.
Future of anesthesiology
Advances during the last several decades have led to important improvements in clinical monitoring technology and clinical practice development, not only in patients undergoing surgery or in patients being cared for in intensive care units but also in ambulatory patients. These developments have contributed to great improvements in patient safety. In addition, anesthesiologists worldwide have developed standards for continuous real-time monitoring of hemodynamics, oxygenation, ventilation, neurological status, urine output, core temperature, degree of neuromuscular blockade, as well as other items, all of which have also contributed significantly to patient safety.
The main avenues where technology is helping reshape medicine can be broadly divided into the artificial intelligence, robotics, nano-medicine, and the genetically targeted medicine.
The concept of AI stems from the superiority of computers at performing repetitive tasks, whereby humans are prone to suffer from tiredness, loss of attention, and boredom. There is an exponential superflux in affordable computational power, and mass accrual of big data has made it possible to develop and propagate deep machine learning algorithms. These algorithms, when applied through reasonable computational power, can perform analyses and tasks at a small fraction of time taken by conventional methods.
It is unclear if AI would obviate the need for having human doctors at some point in future; however, it has outperformed the latter using some specific bench-marks in some specialties. This is particularly true for the disciplines not requiring a degree of emotional intelligence. For example, IBM Watson system has been employed for clinical decision support, and is outperforming human diagnostic capabilities in autism, pneumonia, and in predicting heart attack and stroke. Other software are already performing better than human doctors in interpreting radiological images, and diagnosing skin cancer.
Internet-of-Things(IoT) is bringing the patient – healthcare provider interaction to a whole new level. It is now possible to have a completely patient centered service provision. The patients would be continuously monitored from the comfort of their home, or even on the move, connected to the healthcare providers through, for example, their smartphone, or their smart car. Their compliance with the prescribed level of exercise, food and medicine intake, etc. can all be monitored with appropriate prompts and suggestions issued automatically as needed. If their medicine cupboard is running low on supply, replacement could automatically be requested from their doctor/pharmacy. If they develop a condition, such as a dysrhythmia, first aid including automated electronic defibrillator could be dispatched to their location, ambulance service notified, and the hospital bed prepared for them, all by their smartphone.
In the field of telemedicine, a step ahead from tele-monitoring, the automated critical care system (ACCS) is being trialed by the US Navy, and the system for maintenance of intravenous anesthesia for battle casualties developed by the US Army (AutoTIVATM) is awaiting FDA approval. These systems mean a critically injured patient could be looked after either fully autonomously, or in assist mode by a physician hands-off from a remote location, while awaiting transfer to the healthcare facility, or in transit.
Augmented reality is changing the way medicine is taught, and how surgical procedures are explained to the patients. With the passage of time, experts are expecting to see a continuation of exponential progress in AI ability to perform more tasks with improving proficiency.
Development of robots with fine motor capabilities has made possible the operative techniques, and precision surgery with minimal access, which were previously considered very difficult. In addition to surgery, those are being trialed for other interventional and anesthetic procedures, such as endotracheal intubation, intravenous and central venous cannulation, nerve blocks, resuscitation, and automated drug delivery systems, etc.
Nano-medicine is the field dealing with repairing, constructing, monitoring, and controlling of human biological systems at the molecular level, by applying engineered nano-devices, nano-robots, and nanostructures. It is commonly dubbed as swallowing a doctor. Almost 100 FDA approved nano-molecules are already in practice, and twice that undergoing trials. The volume of sales of nano-medical products is expected to expand from the current level of USD 150 billion, to almost USD 300 billion by 2022.
Nano-medicine is developing mainly in the directions of drug delivery, in-vivo imaging, and developing novel therapies. Some examples include delivery of some cancer drugs by nano-particles, whereby cancer cell specific antibodies locate and enter the target cell and deliver the toxic payload. In vivo MRI image enhancement is achieved by Quantum dots, which have light emitting properties. C-dots (Cornell dots) are infused with organic dye, which will light up with fluorescence, helping surgeons to see the illuminated cancer cells and remove those completely. Dendrimers are being studied for drug delivery, gene delivery, nano-sensors, dye enhancement, blood replacement, etc. Blood purification may be achieved using magnetic nano-particles (Dynabeads) which can bind target molecules (toxins, proteins, pathogens, etc.) and help remove them magnetically. Nano-robots are being trialed for introduction into the body through a syringe and perform selective precision surgery internally.
Genomic medicine is helping define the inter-racial, and even inter-individual, differences in pharmacokinetics, and pharmacodynamics of a given drug. The objective of genomic medicine is self-programming through the microbiome for precision medicine. The human genome project managed to decode approximately 92 percent of the genome, and the testing kit has become very affordable. However, progress on the development of personalized drugs and their dosing has been rather a bit slow.
All above developments collectively imply a reduction in global disease burden, functional medicine promoting health at pre-morbid stage and reducing progress to becoming actually sick, and the technological progress reducing the overall numbers of surgical procedures as well as the actual human input in performance of those procedures. Within our lifetimes one can expect these technologies to replace the surgical and anesthetic workforce, or take on a significant role in assisting them reducing their numbers required.
This has prompted the luminaries in the field of anesthesia to suggest expanding anesthesiologist role from the operating room in to a new discipline: the perioperative medicine, with a broad involvement in anesthesia assessment before surgery, exercise testing and preparation for surgery, enhanced recovery after surgery, and integrated care for the elderly, as a few examples.
Way forward
Technological advances have helped improve safety and quality of anesthesia, and are paving the way to semi-autonomous or even possibly completely autonomous surgery and delivery of anesthesia. Advances in other realms of medicine are improving overall state of health, and reducing the numbers and types of surgical procedures required, thereby reducing the numbers of the relevant workforce, including anesthetists, in future. It is of paramount importance to brace these changes, and transform the specialty of anesthesia into a more over-arching role of perioperative medicine in order to stay relevant.
Industry Speak
An Expansive Product Range And An Equally Impressive Base
Aditya Kohli
Director – Sales & Marketing
Allied Medical Limited
Technology is the way forward. It is one of the most critical tools to measure development as well as progress. Increase and boost of life expectancy is a primary indicator of both. The parameters of progress have hugely evolved too. From medical science to daily living, impact of technology is evident in every sphere of life. Redundancy has become the new fear as well as motivator. What gets redundant gets out of business. In such striving times, it is most wise to invest in equipment that not only meet the technological advancements and innovations but are viable for long-run, in terms of dependable service back-up and utility of usage.
Anesthesia markets have hugely evolved with the rise in various types of surgeries world over. A striking name in such segment for the longest time has been Allied Medical Limited. The company is backed by a strong R&D team that relentlessly innovates and executes. A state-of-the-art manufacturing facility not only readies an expansive product range but is also ready for innovations.The facility is recognized by the Ministry of Science & Technology (Government of India). The company’s stronghold lies in the after-sales service that is not only prompt but solution-bound too.
The company has been closely supporting all leading medical institutions across the country by providing reliable and dependable quality equipment. Our wide product range includes anesthesia machines and workstations, patient monitors, ICU ventilators, infusion pumps, ECG machines, defibrillator, AED, emergency ventilators, OT tables and lights, ICU beds, crash carts, and suction machines. Other than an impressive product portfolio, our most prompt and professional customer support is what sets us apart from our peers. In last so many years, owing to insistence by our clients, we have adapted and engineered ways to provide product services for equipment made by our competitors. This is one of the boldest compliments we continue to receive from a client base spread across the country.
Industry Speak
Technological Advances And Emerging Trends
S Benedict Biju
GM – Respiratory Management Systems
Skanray Technologies
An anesthesia machine is used to deliver fresh gas flow of medical gases like nitrous oxide, oxygen, and inhalational anesthetic agents to induce and maintain anesthesia for a patient during surgery. Starting from the invention of a simple Boyle’s Apparatus in 1917, the method of anesthesia delivery has gone through significant technological advancements over a period of 100 years. The focus is always on making anesthesia delivery much more efficient by reducing use of anesthetic agents as much as possible and still maintaining optimal sedation for the patient. The innovations in the development of sub-systems of anesthesia delivery like ventilator, vaporizer, digital rotameter, circle absorber, and patient monitors are the emerging trends in the anesthesia space.
Now, the technology is advancing toward having all these modules seamlessly integrated into a single entity called anesthesia workstation. It helps clinicians to provide comprehensive care to patients. The evolution of mechanical ventilation technology to address complex lung conditions has contributed to better gas delivery in anesthesia ventilators. Starting from a simple flow divider mechanism to deliver fixed tidal volumes, the latest ventilators can deliver gas in various flow shapes to ensure lowest mean airway pressure, thus reducing the possibilities of volutrauma and baratrauma.
The innovations in the field of anesthetic agents and vaporizers are highly commendable. Starting with ether as the first volatile agent in 1847, now there are numerous anesthetic agents including isoflurane, sevoflurane, and desflurane, which are widely used. Simultaneously, the technology of vaporizers has also grown to administer these anesthetic agents in the lowest possible concentration, thus helping patients to recover faster after surgery.
The future is promising for advanced technologies in the domain of patient monitoring during anesthesia. Various technologies like neuro-muscular transmission (NMT), BiSpectral Index (BiS), and anesthesia gas module (AGM) are increasingly used today. The effort here is to define a spectrum that can be used universally to monitor and maintain adequate depth of anesthesia during surgery. By customizing anesthesia delivery with BiS monitoring, anesthetists are already recording a reduction in use of anesthetic agents up to 50 percent when compared to conventional systems. The benefit is evidenced with better turn-around-time of patients in intensive care units post-surgery. It also helps to reduce our foot-print on global warming which is the need-of-the-day.














