Endoscopy Equipment
Endoscopes Gaining a Technical Edge
The future has many names. Specifically, for endoscopy, AI means a huge opportunity to facilitate endoscopic procedures in the near future.
Over the years, medicines and the way physicians approach the patient have evolved from the basic clinical situations and the way they interpret signs and symptoms to imaging technologies that help them provide a faster and more reliable diagnosis. Nonetheless, along with endoscopy appearance in daily practice, patient’s survival rate and treatment have improved, and have gradually become the mainstream of current use by introducing screening programs, as in colorectal cancer. Based on the perceived balance between the necessity and benefits of endoscopy, this technique has prompted its need to be kept in current practice and has become a benchmark for human organs or cavity exploration. A large array of therapeutic alternatives has positioned endoscopy as the cornerstone for most of the diseases of the gastrointestinal tract and gradually has become a technique that may obviate surgery in some situations. From basic tissue harvesting to real-time confocal microscopic assessment or from palliative therapeutic armamentarium to procedures more closely tied to surgery procedures, gastrointestinal endoscopy has become more and more popular, and along with its advantages or challenges has penetrated the gastroenterology community, becoming the touchstone for this medical specialty.
Modern gastroenterology is based on the availability of endoscopy and its secondary features in assessing the gastrointestinal tract. Technological development is a continuous process in day-to-day life and has been gradually inserted into endoscopy advances along with high-resolution endoscopes, devices, or accessories. The fact that some organs could have only been accessed by surgical procedures has promoted endoscopy to a level worthy of further appraisal. Among the different steps in endoscopy, the ones that surely changed the way physicians tend to diagnose or treat patients in daily practice are endoscopic retrograde cholangiopancreatography, capsule endoscopy, and endoscopic ultrasound. Thus, a new window has been opened for both patients and physicians that allows the concept of evidence-based medicine to be used in daily practice.
Perhaps the biggest effort in endoscopy was to improve the diagnosis of gastrointestinal tumors. With various methods, which are certified for cancerous gastrointestinal lesions, endoscopy has also become a valuable asset for early-stage diagnosis and is still exploring new therapeutic avenues. Endoscopy screening and treatment of pre-cancerous lesions is part of a growing trend that has been increasing exponentially in many specific lesions due to new technology embedment or transposing current surgical procedures. Thus, a shift has taken place and the use of endoscopic systems has allowed technology to become part of both the physician’s and the patient’s life.
Indian Market Dynamics
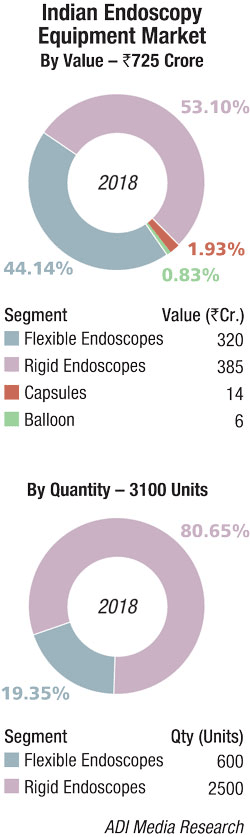 The Indian endoscopy equipment in 2018 is estimated at Rs 725 crore, with the rigid endoscopes segment estimated at Rs 385 crore and the flexible endoscopes segment at Rs 320 crore. Capsules contributed Rs 14 crore and balloon another Rs 6 crore. In unit terms, it is estimated that in 2018, 600 numbers of flexible and 2500 numbers of rigid endoscopes were sold in the Indian market.
The Indian endoscopy equipment in 2018 is estimated at Rs 725 crore, with the rigid endoscopes segment estimated at Rs 385 crore and the flexible endoscopes segment at Rs 320 crore. Capsules contributed Rs 14 crore and balloon another Rs 6 crore. In unit terms, it is estimated that in 2018, 600 numbers of flexible and 2500 numbers of rigid endoscopes were sold in the Indian market.
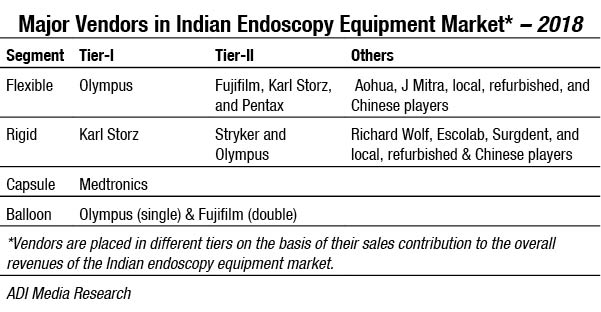
The flexible segment is dominated by Olympus, with Fujifilm, Karl Storz, and Pentax being aggressive players. Other players include Auhoa and J Mitra.
Karl Storz, Olympus, and Stryker are aggressive players in the rigid category. Other brands which are present are Richard Wolf, and Surgdent.
Capsule endoscopes are dominated in India by Medtronics, although globally some of the notable industry players include Olympus Corporation, CapsoVision, Chongqing Jinshan, RF System, Fujifilm, Given Imaging Ltd. and IntroMedic.
Balloon assisted enteroscopy allows advancement of a long endoscope into the small intestine for both diagnostic and therapeutic purposes. Physicians use balloon-assisted enteroscopy for conditions affecting both the upper GI tract and the lower GI tract. This procedure can effectively provide access to the small intestines, which is very long, which makes it difficult to access using other procedures. This technology allows gastroenterologists to conduct biopsy, remove small bowel polyps or a foreign object and even enlarge a narrowed stricture in the upper or lower GI tract. Balloon-assisted enteroscopy is sometimes also conducted alongwith capsule endoscopy to get a better view of the area needing treatment. In India, double balloon enteroscopy is catered to largely by Fujifilm and the single balloon enteroscopy largely by Olympus.
The small intestine, which used to be called the dark continent was long regarded as being difficult to diagnose and treat due to challenges with endoscope insertion. Balloon endoscopes and manually operated spiral overtubes that appeared in the 2000s made it possible to shorten the small intestine by pleating, which made deep enteroscopy easier. However, many of these systems require two operators and can be very difficult to operate, often resulting in long procedure times. In order to overcome these challenges, in 2011 Olympus wholly acquired US-based Spirus Medical, which possessed special technology for motorized spiral overtubes. By integrating this technology with its own, Olympus has now developed the new PowerSpiral enteroscopy system. In March 2019, Olympus launched this product in Indian hospitals.
 In February 2019, Aohua announced its Indian marketing service center in Mumbai, in anticipation that the Indian market’s demand to increase for endoscopic diagnosis and treatment over the years.
In February 2019, Aohua announced its Indian marketing service center in Mumbai, in anticipation that the Indian market’s demand to increase for endoscopic diagnosis and treatment over the years.
Asian Institute of Gastroenterology, Hyderabad procured endoscopes for about Rs 25 crore in 2018. Since the facility established as a new concept of day care unit where major endoscopic surgical procedures could be done on an outpatient basis without resorting to hospitalization. Since then the institute has become one of the largest referral centers in Asia for Therapeutic Endoscopy. Patients are referred from not only most cities in India but also from surrounding countries like Sri Lanka, Bangladesh, Malaysia, and Nepal.
Global market
The endoscopy devices market, which was valued at USD 25,273 million in 2018, is expected to register a CAGR of about 6.45 percent during 2019 to 2024, forecasts Mordor Intelligence.
Technological advancements, such as adoption of near-infrared radiation technology (NIR), flexible spectral imaging color enhancement (FICE), I-scan technology, confocal laser endomicroscopy (CLE), and computer-aided detection systems are enhancing the diagnostic and therapeutic use of endoscopy. The CLE technology is being developed by Mauna Kea Technologies (France), which combines the microscopy and endoscopy technology to produce images (optical biopsies) that eliminate the need of tissue biopsies and aid in immediate informed decision making.
Vendor updates
In June 2019, to enable upcoming regulatory filings, Medtronic plc made public its partnership with Karl Storz SE & Co. KG. For the past 4 years, the two companies had partnered to seamlessly integrate Karl Storz’s three-dimensional (3D) vision systems and visualization components into Medtronic’s forthcoming robot-assisted surgical platform.
In March 2019, Olympus Corporation announced the launch of PowerSpiral in Europe and parts of the Asia-Pacific region, including Hong Kong and India. The system uses a motorized rotating attachment that mounts on the scope and gently grips onto the mucosa to help the endoscope advance deep into the small intestine. Going forward, PowerSpiral is planned for a launch in the United States and other parts of the Asia-Pacific region as regulatory procedures are completed. The product is an endoscopy system designed for diagnosing and treating conditions of the digestive tract. It incorporates the world’s first foot-switch-operated motor that rotates an overtube equipped with spiral-shaped fins positioned on the endoscope. The rotation of the spiral fins supports continuous pleating or folding of the intestine, with a goal of improving scope maneuverability and shortening procedure times. In May 2018, the company had announced the launch of the ENF-VT3, the world’s first rhino-laryngo videoscope to incorporate 4-direction angulation capability, initially on European market in the beginning of June, and on Japanese market, followed by the markets in the rest of the world. Rhino-laryngo videoscopes are usually inserted via the nasal cavity and used to examine the pharynx and larynx. They can also be used together with endotherapy devices to perform procedures such as the extraction of foreign bodies, resection of vocal cord polyps, or injection into the vocal cords.
In October 2018, Fujifilm India Private Limited launched Eluxeo 7000 series, a range of novel image-enhanced endoscopy products, which have blue-light imaging (BLI)/Linked color imaging (LCI) technology to help aid early detection of all types of gastro cancers. This will help the company to strengthen its foothold in the medical business in India. The Eluxeo 7000 Series increases the survival rates by early detection of gastrointestinal (GI) cancer.
The Eluxeo 7000 series brings in LCI technology that differentiates the red color spectrum more effectively than white-light imaging. The increased color contrast improves detection of inflammation and results in more accurate delineation. BLI on the other hand, with its high-intensity contrast imaging allows superior visualization of superficial vascular and mucosal patterns, thereby ensuring early detection of cancer lesions.
In 2018, Pentax had continued with its acquisition spree. In August, the company announced that it had acquired a controlling interest in PlasmaBiotics SAS, based in Paris, France – a company that designs, manufactures, and markets devices for drying and storage of endoscopes. The investment in PlasmaBiotics strengthened Pentax Medical’s hygiene portfolio and its continued focus on reducing cross-contamination risks to enhance patient safety in endoscopy. In July 2017, Pentax had announced the creation of a joint venture to develop products in the field of flexible medical endoscopy. The vendor in January 2017 had acquired C2 Therapeutics, strengthening its therapeutic endoscopy portfolio.
Buying new versus refurbished units
- The pros of buying new systems include:
- New equipment is the best way to tap into the most current technologies in the market;
- Extended warranties and factory service agreements; and
- Financing options.
Some cons of buying new systems can be:
- Higher initial acquisition cost;
- Possible limitations on where equipment can be serviced; and
- May need to upgrade additional equipment, such as video towers, mating instrumentation if new models are not compatible with existing equipment you had planned on keeping.
Pros of buying refurbished systems:
- Substantially lower acquisition cost in many cases;
- Can acquire through an OEM or reputable re-seller;
- Some resellers offer financing;
- One can add additional equipment compatible with their existing video equipment and instrumentation; and
- Wide range of service options from ISO.
Some cons of buying refurbished systems:
- Older technology that is closer to obsolescence;
- Possible variances in equipment condition; and
- Due diligence is required to find a reputable re-seller – look closely at credentials, years in business, expertise, and online ratings.
Generally, to get the most for money, buying refurbished products can save the average buyer between 40 and 80 percent on price. However, because endoscopes
are fragile, buying new ones is sometimes a safer option, so one can guarantee the quality and care of the endoscope throughout its lifespan. While it might be more money upfront, the equipment will pay for itself over time.
Buyers’ perspective
High-quality surgical equipment and specialty endoscopes represent a significant investment for healthcare providers, so it is important to recognize that selecting and working with the appropriate vendor when making endoscope purchases and service decisions can pay off in the long run. Another essential part of this process is for customers to fully assess the total cost of ownership of endoscopes being purchased. It is equally important to understand that the repair and service of this costly, delicate equipment represents a critical component of the total cost of ownership.
When purchasing an endoscope, buyers should keep renting or financing options in mind – especially if they are a new buyer. Some endoscopes can cost upwards of USD 10,000, so while it is usually preferred to buy new, that is not always possible. Additionally, buying multiple pieces of equipment from the same company can save time and money. Rather than spreading equipment purchases among several companies, by purchasing from one company, buyers are more likely to receive preferred pricing, convenient installation, and other value-added services.
Technological advancements
In the age of smartphones and wireless communication, endoscopists across the globe look to future trends in endoscopic technology. There is no doubt that technology is rapidly evolving with ever-increasing connectivity amongst individuals, institutions, and even nations. Yet, designing a state-of-the-art endoscopy suite remains a challenge when it comes to integrating devices with all the different software platforms required to perform a procedure, capture images, monitor quality metrics, track scope reprocessing, and ultimately achieve the desired outcomes, which are ensuring accuracy and patient safety.
Device-assisted enteroscopy. Development of endoscopic methods for evaluation of the small bowel started almost simultaneously with flexible colonoscopy. First successful total enteroscopy was reported in 1971, using a ropeway and also a sonde method. However, both methods were cumbersome, time-consuming, and technically challenging, and thus did not achieve wide acceptance in clinical routine. For approximately 30 years, push-enteroscopy was the preferred method, leaving the deep portion of the small intestine invisible and inaccessible to endoscopic evaluation. The advent of video-capsule endoscopy (VCE) as a novel non-invasive and reliable method for visualization of the entire mucosal surface of the small bowel in 2000 led to a substantial change in diagnostic assessment of patients with suspected small bowel disorders. The development of device-assisted enteroscopy (DAE) in 2001 established a practical method for examination of the small bowel and resulted in a paradigm shift in diagnostic and therapeutic approach in patients with suspicion of small-bowel diseases. Currently, three platforms for deep enteroscopy exist: double-balloon enteroscopy, single-balloon enteroscopy, and spiral enteroscopy. Balloon-guided enteroscopy is not well established in clinical routine, despite a few published trial reports, a diagnostic yield, and DMI not inferior to standard DAE. The double-balloon and single-balloon enteroscopy systems are the most commonly used devices in Europe. After thorough clinical evaluation, SE has gained wide acceptance in North America but less in Europe. Despite these substantial improvements in the field of direct enteroscopy, even nowadays deep endoscopic access to the small bowel with all available methods is still a complex procedure – cumbersome and time-consuming and requires high endoscopic skills. Thus, the technique of deep enteroscopy was further developed. In November 2015, clinical evaluation of a novel motorized version of the SE system started with the first in human case of PowerSpiral enteroscopy being performed. The role of small-bowel capsule endoscopy and DAE for diagnosis and treatment of small-bowel disorders was recently addressed in clinical guidelines and technical reviews by the European Society of Gastrointestinal Endoscopy, American Society of Gastrointestinal Endoscopy, and Japanese Gastroenterological Endoscopy Society.
Balloon-assisted enteroscopy. This is an incisionless procedure performed to reach and treat less-accessible colon polyps or areas of bleeding in the gastrointestinal (GI) tract. During the procedure, gastroenterologists use flexible, tube-like imaging instruments to see the area of the body being treated. Balloon-assisted enteroscopy uses endoscopes equipped with balloons that inflate and deflate to pinch together the walls of the GI tract. By compressing the walls, the gastroenterologist can reach and treat less accessible areas. The enteroscopy may be done as an inpatient or outpatient procedure. Eligible patients can avoid surgery and may recover faster.
Endoscopy robotics. Many different types of endoscopy robots have been developed or are under development. Some of these innovative biotechnologies are dedicated to complex endoscopic procedures, such as endoscopic sub-mucosal dissection whereas others are purely diagnostic. In endoscopy robotics, there are still several problems that need a solution. These problems basically concern robotic locomotion and instrument control, as well as clinical applications. In most cases, the technology is still under development. The current fields of investigation are augmented reality, advances in actuation and reduction of hysteresis, optical analysis, wireless movement transmission, and many others. Besides endoscopic sub-mucosal dissection, other promising fields of implementation of endoscopy robots are natural orifices transluminal endoscopic surgery and bariatric endoscopy.
Within the next 5 years physicians will be able to use robotic endoscopy to remove potentially cancerous lesions during colonoscopy instead of referring patients for colectomy. And over the longer term, perhaps over more than a decade, patients will be able to undergo endoscopic removal of those lesions during colonoscopy instead of being referred.
Obviously, endoscopy robots are expensive, but both doctors and health-system providers are becoming more aware of the possibilities that these platforms can offer. Improvement of the performance of endoscopy robots undoubtedly will lead to their widespread use and, therefore, a balance in cost‐effectiveness.
Endoscopic ultrasound. Endoscopic ultrasound (EUS) development has opened up new horizons for diagnosis and management, especially in pancreatobiliary disease. On a continuous evolution process, EUS has been introduced as a standard diagnosis technique, which provides information of structures located near the gastrointestinal tract. The arrival of fine-needle aspiration (FNA) has paved the way for various new therapeutic options that may substitute several surgical procedures or provide new options for cancer therapies. EUS-drainage of fluid collections represents the grounds for novel techniques, which focus on joining two cavities. Along with the additional growth of the industry of endoscopy supplies, EUS has enabled novel therapeutic alternatives.
Confocal laser endomicroscopy. CLE is a cutting-edge technique based on real-time image reconstruction on a subcellular level, in any endoluminal cavity by using flexible endoscopy. The ability to see the microarchitecture in vivo in a non-invasive setting has opened up new windows of opportunity for a faster diagnosis. Thus, providing images of the mucosal layer will not only ensure a rapid assessment of the lesions, but will also have a role in choosing the right therapeutic management. Based on a low-energy light source that enables acquisition of histology-like images, CLE usually requires the use of a dye for a better characterization of morphology or vascular pattern. CLE is considered a valuable tool with great potential that may overcome some of the disadvantages of classic histology such as time waiting or sampling bias, thus facilitating live diagnosis and treatment decisions. Also, its use might also lead to a lower number of biopsies, provide a real-time differential diagnosis in pancreatic tumors or access to the biliary tree, or even reduce the number of noncancerous lesions removed through endoscopic procedures.
Next generation of endoscopy technology. Biotechnologists, physicists, and medical researchers at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) have developed technology for microscopic imaging in living organisms. A miniaturized multi-photon microscope, which could be used in an endoscope in future, excites the body’s own molecules to illuminate, and enables cells and tissue structures to be imaged without the use of synthetic contrast agents. Multi-photon microscopy offers decisive advantages over conventional methods. Patients do not need to take synthetic contrast agents for the imaging of parts of connective tissue as the body’s own markers illuminate due to the excitation by photons. In addition, the multi-photon laser penetrates deep into cells, for example, into the walls of the colon, and provides high-resolution three-dimensional images of living tissue, whereas conventional colonoscopy is restricted to images of the surface of the colon. The procedure could supplement biopsies or even make them superfluous in some cases. Multi-photon microscopes are already in use in medical applications, especially on the surface of the skin. For example, dermatologists use them to look for malignant melanoma. The challenge for using these microscopes in endoscopic examinations is the size of the technical components. Researchers at FAU have now successfully managed to house the entire microscope and femtosecond laser in a compact, portable device. The objective lens is housed in a cannula that is 32mm long and has a diameter of 1.4mm. The focal point can be adjusted electronically to vary the optical penetration. A prism is located on the point of the needle, allowing a sideways view into the colon, which means various rotational images of the tissue can be made from the same position.
In current experiments on small animals, the light emitted from the laser is transmitted via a rigid system. More research is needed to integrate the system into an endoscope. Special photonic crystal fibers are required to guide the laser pulses, Furthermore, in addition to the objective lens, the entire scanning mechanism must be miniaturized to allow it to be integrated into a flexible endoscope.
Multi-photon microendoscopy is not only useful for examining the colon, it could also be used in other areas of the body, such as in the mouth and throat or in the bladder. The aim of the new method is to enable the doctor to detect whether organ cells and parts of the cell wall have changed on the micrometer scale. Complex dyeing processes and time-consuming biopsies can thus be limited. Prof. Friedrich’s team aims to provide doctors with an image database providing a multi-photon atlas of organs and various diseases.
Outlook
Applications of AI techniques, specifically machine learning and more recently deep learning, are beginning to emerge in GI endoscopy. As applications of artificial intelligence in gastroenterology continue to increase, there are several areas of interest that will hold significant value in the future. First, the technical integration of AI systems with existing electronic medical records (EMR) and endoscopy platforms will be important to optimize clinical workflow. New AI applications must be able to easily read in data from a video input or EMR, allowing the systems to use the data for training and real-time decision support. A seamless integration in the endoscopy suite will be crucially important in encouraging clinician adoption.
Second, AI systems must continue to expand their library of clinical applications. There are several promising studies that demonstrate how AI can improve performance on clinical tasks such as polyp identification, detection of small-bowel bleeding, and even endoscopic recognition of H. pylori and hookworm infection. Future research should continue to identify new clinical tasks that are well-suited to machine-learning tools.
Third, further research is needed to understand the ethical and pragmatic considerations involved in the integration of artificial intelligence tools in gastroenterology practice. To begin with, what is the general physician sentiment toward AI? Is AI considered a threat or a tool by the gastroenterology community? A deeper understanding of the end user is crucial to dictating how these tools should be designed and deployed. If AI tools are accepted by physicians, how will experts train individuals to use these technologies effectively? Will the learning curve for using these systems be prohibitive? If so, further research is needed to describe the most effective training methods for physician practices beginning to adopt AI technology. In today’s technology-driven environment, it is clear that data security is of utmost importance, especially when dealing with protected health information. As the number of AI tools increases, so too should efforts toward designing security systems and encryption methods to safeguard clinical data. Finally, the clinical community needs to decide on standards for approval and regulation of new AI technologies, including potential implications for legal matters including medical malpractice.
As the field evolves, a watchful eye is needed to ensure that security, regulation, and ethical standards are upheld.
Second Opinion
 Dr Naresh Bansal
Dr Naresh Bansal
Gastroenterology, Hepatology,
and Endoscopy Specialist,
City Hospital
Endoscopy fast replacing surgery
There was a time when endoscopes were used mainly for diagnostic purpose. They were rigid and difficult to maneuver. Then flexible endoscopes and compatible accessories made advances in therapeutics. Endoscopes were being used to cease bleeding, take biopsies, and cut polyps. Argon plasma coagulation, banding of varices, application of injections, and removal of foreign bodies became possible with innovations in accessories. Cautery and special dedicated instruments made ERCP possible. Small bowel was still out of reach of the endoscopists. Then advent of balloon-assisted enteroscopy and capsule endoscopy made this possible.
Introduction of EUS gave the power to visualize outside the lumen. A range of procedures, which were only possible through surgery, thus became possible with just endoscopic route, bringing down the cost of the procedure and making the whole procedure simple to the patient.
The latest is the third-space endoscopy. Procedures like POEM (per oral endoscopic myotomy, to treat achalasia, a condition which leads to difficulty in swallowing due to tight lower end sphincter of food) and ESD (endoscopic submucosal dissection, to remove submucosal tumors and early cancers through endoscopy only) changed the entire paradigm. Recently, we removed an 8-cm polyp from stomach with endoscopy, which otherwise was impossible few years back. CO2 insufflators made the long procedures easy as distension was less with CO2. Availability of covered stents, over the scope clip and full thickness sutures, changed the trend we used to seal holes or perforations in intestine.
Another front where endoscopists are replacing surgeons fast would be management of obesity. Now various procedures to treat obesity can be done by endoscopy only without surgery, and this is going to be huge success in the near future.
Endoscopy has a bright future and it is progressing fast horizontally and vertically. This is going to foster the demand for equipment and accessories. The need of the hour is to develop right equipment at the right cost. This requires basic R&D in India itself for bringing down the cost. It will make latest innovations more acceptable and popular among endoscopists and general public. The instruments should be reliable, affordable, and of good quality. The field is poised to growth undoubtedly. Endoscopy is changing the perspective, evolving rapidly, transforming entire medical field silently, and encroaching the surgeon’s space slowly but definitely. A lot of innovations are yet to be done and the industry should be ready for it.












