MRI Equipment
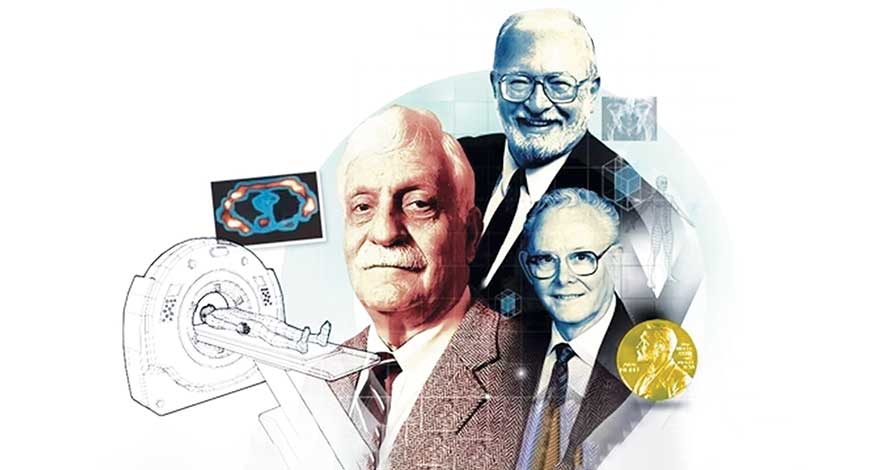
MRI | A 50-year journey
The transformative evolution of MRI over five decades, with their profound impact on diagnostic imaging and healthcare.
Fifty years ago, a scientist named Paul Lauterbur wrote a paper that showed a new way to look inside the human body using a technique called magnetic resonance imaging, or MRI. Instead of using x-rays like traditional methods, MRI uses strong magnets and radio waves to create detailed pictures of the inside of our bodies.
For his groundbreaking work in developing MRI technology, Lauterbur He won the 2003 Nobel Prize in Physiology of Medicine for developing MRI with Sir Peter Mansfield, a British physicist.
Since that time, MRI has become an essential tool for doctors to view inside the body and see soft tissue like the heart, brain and other muscles and organs. MRI images help doctors understand what is happening in disease. MRI lets you view the status of tissue, observe shapes, blood flow, inflammation and even the changing shape of soft tissue. Because MRUI enables doctors to look inside the body quickly and clearly, advanced treatments have been developed which has led to longer, healthier lives.
MRI is a flexible imaging technique, and MRI scanners have continued to improve over the years. The unit of measure for magnetic field strength is Teslas. The earth’s magnetic field is approximately 0.00005 Tesla. Lauterbur’s first human MRI magnet was 0.09 Teslas. That’s about 2,000 times the earth’s magnetic field. He was able to see structures in the body, but the resolutions were grainy and at low resolutions.
Today’s MRI systems are 1.5T, 3T, but recently an MRI magnet that’s 7 Tesla was purchased by the University of Illinois Urbana-Champaign and Carle Hospital. It’s 75 times stronger than Lauterbur’s original magnet and allows us to localize function in the brain down to 0.5 millimeters with clarity and excellent contrast.
The advent of portable MRI scanners represents a significant leap forward in medical imaging technology, promising a multitude of benefits for healthcare systems worldwide. These innovative devices, distinguished by their compact size and mobility, herald a new era of convenience and accessibility in diagnostic imaging. By virtue of their portability, these scanners can be seamlessly integrated into various clinical environments, from bustling hospital wards to remote clinics in underserved communities. This capability to bring advanced imaging technology directly to the patient’s bedside holds immense potential for improving healthcare delivery.
Furthermore, the affordability of portable MRI scanners makes them an attractive option for healthcare facilities with limited resources, both in developed and developing regions. This democratization of medical imaging technology has the potential to bridge existing disparities in access to healthcare services, ensuring that individuals from all walks of life can benefit from timely and accurate diagnoses.
Despite their compact design and lower magnetic field strength compared to traditional MRI machines, portable scanners are capable of producing clinically relevant images that facilitate informed decision-making by healthcare professionals.
While challenges such as image resolution and data interpretation persist, ongoing advancements in technology and image processing algorithms hold promise for addressing these limitations. As these portable MRI scanners continue to evolve and gain acceptance within the medical community, they have the potential to revolutionize healthcare delivery by expanding access to high-quality diagnostic imaging services and improving patient outcomes on a global scale.
Traditionally, MRI is not practical as a POC tool since the high magnetic fields (typically 1.5–3 Tesla) needed for operation present a projectile hazard for ferrous objects if operated outside of an access-controlled scanner suite. Additionally, the need for magnetic and radio frequency (RF) shielding, as well as power requirements that can exceed 25 kW, increase the footprint precluding use at the POC. It is also not compatible with patients that have certain types of metal implants; the high cost of scanner purchase and site infrastructure limitations prevent many facilities from having multiple scanners, limiting capacity despite high demand for instrument use.
Recent technical innovations in MRI physics and instrumentation have led to scanners operating at far lower magnetic fields than previously thought possible and have enabled 64 mT MRI scanners to be deployed at the patient bedside for POC use. These low-cost low-field MRI scanners can operate without the shielding and safety requirements of traditional high-field scanners, but their use to date has focused on neuroimaging in critical-care settings.
Single-sided magnetic resonance (SSMR) sensors may provide a portable POC diagnostic option that leverages the power of MR-based contrast with purpose-built low-cost hand-held instruments. These devices use magnetic resonance techniques to acquire spectroscopic (i.e., non-imaging) data over a limited tissue depth but have the ability to distinguish between tissue types, intra- and extra-cellular compartments and provide information about tissue architecture. Analysis spatially resolved T2-relaxation data from MRI has shown that the skeletal muscle compartment and the subcutaneous compartment can be represented by biexponential decays. There is extensive evidence of skeletal muscle quantitative T2 relaxation being better represented by a bi-exponential model as compared to a mono-exponential model.
Techniques including T2 relaxometry and T2-weighted diffusion can be performed on single-sided sensors to provide clinically-actionable information. Uses include assessment of liver disease, inflammation, tumor characteristics, iron overload, and cartilage diseases, among others. Within skeletal muscle tissue specifically, relaxometry can provide insight into fluid status, progressive disease musculoskeletal disease monitoring (sarcopenia, muscular dystrophies, etc.), vascular kinetics and oxygenation tracking, among other applications.
MRI meets AI
One of the latest enhancements in the MRI field that is not yet fully adopted by hospitals and other healthcare providers is the use of artificial intelligence (AI) to enhance the quality of the scans taken and to provide supportive tools for the more repetitive tasks associated with the MRI process. The use of AI enhances efficacy and boosts efficiency for technologists, leading to faster diagnosis rates, including quicker cancer detection, and earlier intervention.
AI integration, advanced digitalization and the introduction of AI are enhancing the reliability of MRI as a diagnostic tool. AI aids in optimizing MRI scans, improving accuracy, and detecting subtle abnormalities that may be missed by the human eye.
Enhanced cardiac imaging, MRI technology offers detailed cardiac imaging, showcasing cardiac chambers, outflow tracts, and muscle damage from various angles. This comprehensive view provides superior detail compared to other imaging modalities, streamlining diagnosis and potentially reducing the need for multiple diagnostic procedures.
Precise disease detection, AI-powered image processing can identify early-stage cancerous nodules, lesions, and quantify brain scans to detect diseases like dementia and Alzheimer’s. The technology’s precision enhances diagnostic accuracy, potentially leading to earlier intervention and improved patient outcomes.
Virtual reality integration, MRI images can be uploaded to virtual reality (VR) platforms, allowing surgeons to gain additional insights and plan surgical procedures more effectively. VR-based pre-surgery preparation minimizes the impact on organs or tissue during invasive procedures and aids in medical education and training.
AI-based MRI tools are showing promise in the diagnosis and management of multiple sclerosis (MS), a prevalent neurodegenerative and inflammatory condition of the central nervous system. With approximately 2.8 million individuals globally living with MS, accurate assessment and monitoring are crucial for disease management. Traditional MRI methods rely heavily on radiologists’ expertise for lesion detection and analysis, which may limit the detection of subtle changes and impact treatment decisions.
However, AI algorithms offer automation and enhanced sensitivity in lesion detection, providing valuable insights into disease activity and progression. A recent research assesses the accuracy and effectiveness of AI based imaging techniques to diagnose MS. This evaluated the effectiveness of an AI-based tool, iQ-MS, in analyzing MRI scans of MS patients.
This tool demonstrated the ability to accurately evaluate disease activity and lesion burden, offering improved clinical assessment compared to conventional methods. Utilizing deep neural network technology, iQ-MS generates comprehensive data on brain volume changes and lesion metrics, facilitating real-time monitoring and personalized management of MS patients. The integration of AI-based MRI tools like iQ-MS holds promise for enhancing clinical imaging, supporting disease-specific research, and optimizing patient care in MS management.
Outlook
The future of medical imaging holds great promise with the integration of AI and the advent of portable MRI equipment. Such technologies promise to streamline workflow, improve diagnostic accuracy, and facilitate earlier intervention revolutionizing healthcare delivery by increasing accessibility and convenience. As these technologies continue to evolve and gain acceptance, they have the potential to reshape the landscape of diagnostic imaging, ensuring that individuals worldwide receive timely and accurate diagnoses, leading to improved healthcare outcomes on a global scale.














