Nuclear Medicine Equipment
The changing landscape of nuclear medicine

Coupled with AI, nuclear medicine is poised to continue transforming the medical landscape, leading to improved patient outcomes and contributing to the advancement of healthcare.
Nuclear medicine, with its fusion of medical imaging and therapeutic techniques, is reshaping the way diseases are diagnosed, treated, and managed. From detecting early signs of cancer to pinpointing neurological disorders with exceptional accuracy, nuclear medicine is propelling healthcare into a new era of precision and personalized care.
With the rising incidences of these diseases globally, there is a growing demand for nuclear medicine procedures, including PET and SPECT scans. These techniques, have been advancing rapidly and enable the visualization and quantification of molecular processes within the body. In addition, hybrid imaging combines two or more imaging modalities to provide complementary information, and improve diagnostic accuracy. For instance, PET-CT and PET-MRI are commonly used hybrid imaging techniques. These approaches merge functional and anatomical information, providing a comprehensive view of disease processes. Hybrid imaging is particularly valuable in oncology, cardiology, and neurology.
While the potential for nuclear medicine is vast, there are also certain constraints on its widespread adoption. One of the primary challenges is the short half-life of radiopharmaceuticals. Not using radioisotopes within their given shelf-life period leads to radiation and chemical decomposition, lowering radiochemical purity to an unacceptable form, which may prove lethal during diagnosis and therapy. Additionally, the shorter half-life of radiopharmaceuticals creates a need for radiopharmaceutical production in cyclotrons/generators within hospital premises, further increasing the capital expenditure for hospitals.
In addition, nuclear medicine involves the use of complex imaging equipment and radiopharmaceuticals, which can be costly to develop, produce, and maintain. The high up-front costs associated with nuclear medicine equipment and infrastructure can be a significant restraint for healthcare providers or facilities looking to invest in this technology.
Another concern is the limited availability of radioisotopes. Nuclear medicine heavily relies on the availability of specific radioisotopes for various imaging and therapeutic applications. The production and distribution of these radioisotopes can be challenging, and there have been instances of supply shortages or disruptions of certain radioisotopes, such as Tc-99m (technetium-99m), widely used for imaging and diagnostic purposes. Limited availability or inconsistent supply of radioisotopes can restrict the expansion and accessibility of nuclear medicine procedures.
Efforts are being made to enhance the production and availability of radiopharmaceuticals. This includes the development of compact cyclotrons for on-site production of short-lived isotopes, such as fluorine-18, and the use of generator systems to produce longer-lived isotopes, such as technetium-99m.
The problem remains that the world’s research reactors are rapidly ageing and no bullet-proof solution seems to be in sight. With the NRU no longer in operation and France’s Osiris reactor – another key producer of isotopes – also shut down, production capacity has to be met by fewer facilities. With the exception of Germany’s FRM-II and Australia’s Opal, all the reactors used to produce life-saving isotopes have been operating for longer than 40 years. Many could reach the end of their operation before 2030.
A material testing reactor, the Jules Horowitz reactor, has been under construction in southern France since 2007 and is expected to be online in the early 2030s, though the project has seen both delays and cost overruns. The Pallas reactor project in the Netherlands recently received a construction license and will help replace retiring isotope production capacity. It is expected to be online in 2026, and in 2030 it will fully replace the HFR on the same site, which is to be retired. In South Korea, the Kijang research reactor is to be built by the Korea Atomic Energy Research Institute with target deployment in 2027.
The problem for securing future replacement capacity for ageing facilities lies in the fact that the production of medical isotopes was historically not the primary goal of a research reactor, but rather a by-product.
Nuclear Medicine Europe (NMEU), a Brussels-based association for the nuclear medical industry, outlines four main challenges facing Europe’s nuclear medicine sector – secure and reliable supply, regulation, support for innovation and research, and raising public awareness.
The organization of healthcare systems also needs to be re-evaluated to address the skills needed for nuclear medicine, including the development of an expert workforce of oncologists, radiotherapists, nuclear medicine physicians, radiologists, and radio-pharmacists.
Nuclear medicine is witnessing a revolution across a large spectrum of patient care applications, hardware, software, and novel radiopharmaceuticals. It is the most rapidly growing subspecialty in radiology. Over the past 10 years, a variety of tools have started to be incorporated as a standard of care in the nuclear medicine clinic, including wider use of hybrid imaging devices, novel hardware technology, unique crystals, materials, and wider availability of indication-specific radiopharmaceuticals for diagnosis and treatment. More advanced software is being incorporated into the clinic with a variety of commercial vendors modernizing their software platforms and going through the necessary FDA approval process. This encompasses independent vendors as well as scanner based pre- and post-processing workstations, seemingly fancy but very useful and necessary. This has completely changed clinical practice.
An explosion of novel hardware technology has made its way into the clinic, all to the patient’s benefit including total body PET/long axial field of view PET PET/MRI, LINAC PET, total body single photon emission tomography (SPECT), CZT digital SPECT technology, SPECT/MR as well as high-end traditional SPECT/CT scanners. These allow for a personalized approach, using the right tool for the right patient and to optimize radiation doses, acquisition protocols, scanning times, and overall patient care for diagnosis, dosimetry, and treatment.
Major vendors have developed advanced software suites on scanner workstations or independent consoles, as well as online/through cloud systems. Independent commercial software is also now state-of-the-art with advanced processing and post-processing capabilities in SPECT and PET hybrid imaging, as well as incorporating advanced techniques in cardiac, general, musculoskeletal, oncology, neuronuclear, and therapy applications.
Multiprobe assessments for accurate disease characterization. Current clinical paradigm uses a single probe for diagnosis, staging, or other modes of patient care. However, it is quite clear that this strategy is suboptimal and limited as it fails to fully characterize the entire phenotype of the patient’s disease. Multiparametric assessments of disease using multiple probes, advanced image analysis tools coupled to other biochemical, proteomic, and genomic data in the same patient will be incorporated into routine clinical practice.
Dynamic treatment modulation is also necessary. Risk adapted treatments are needed moving away from static systems of clinical care to dynamic systems modulating patient management across the clinical patient historical continuum. Nuclear medicine offers predictive and prognostic biomarkers allowing and contributing to dynamic treatment modulation.
Indian market
The Indian market for nuclear medicine equipment in 2022 is estimated at ₹682 crore, a huge jump from ₹164 crore in 2021. The market had seen a 53-percent decline by value in 2021 over 2020, a direct impact of very low procurement in the pandemic, with budget allocation for healthcare having flowed toward special requirements in the fight against Covid-19 that ranged from ensuring essential medicines to vaccinating the population against the virus. The market in 2023 is heading to close at ₹550 crore, a 20-percent decline.
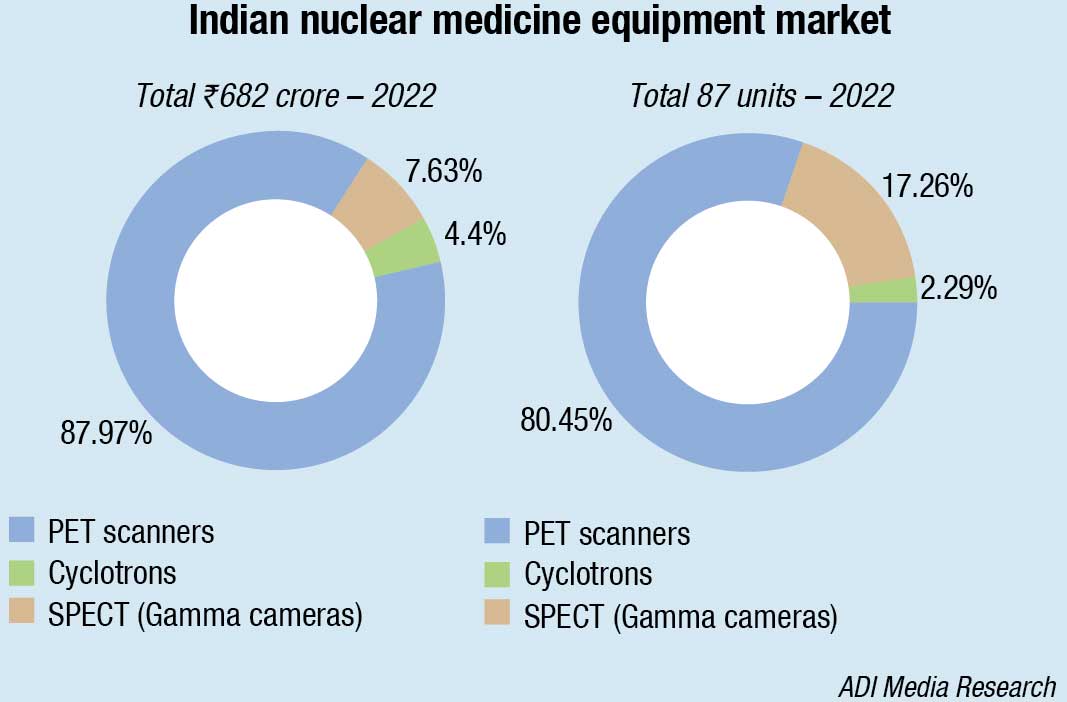
With pent up demand having been met in 2022, the market is stabilizing to a post-Covid annual market in the vicinity of ₹500 crore from a pre-Covid ₹350-crore market. This may be attributed to the dramatic increases in cancer, as 90 percent of the PET scanners that constitute 88 percent of the market by value are used for cancer. Digital PET scanners priced almost twice the analog PET scanner are primarily sold in metros and Tier-I cities.
|
Indian nuclear medicine equipment market Leading players – 2022 |
|
| PET scanners | GE & Siemens; United Imaging |
| SPECT (Gamma Cameras) | GE & Siemens |
| Cyclotrons | GE and IBA, Belgium |
|
ADI Media Research |
|
The single-photon emission computed tomography (SPECT) segment continues to meet the niche demand, with its multiple uses for endocrine, thyroid, ortho, cardiology, neurology, and oncology.
Two cyclotrons were sold in 2022, one by GE to Ruby Hall to the three-member consortium led by Dr Ranjan Kabra in Jaipur, and the second by IBA, Belgium, to Sreeji Diagnostics in Lucknow, average unit price being in the vicinity of ₹15 crore.
Nuclear medicine is giving promising results for patients of prostate cancer, lung cancer, stomach cancer, and other types of cancer where surgery is not an option. However, starting a nuclear medicine department in a hospital or diagnostic center is a humongous effort and investment is quite high. To overcome this, India needs rationalization of resources, subsidization of equipment and radioisotopes, and training of more medical and non-medical personnel in nuclear medicine. This was echoed by doctors at a one-day Conclave on Nuclear Medicine held in New Delhi under the aegis of the Society of Nuclear Medicine.
More than 250 doctors from prominent medical institutes and hospitals across northern India attended the conference. They brought to the fore the concern on the relatively slower growth in the country compared to other branches of medical science, and challenges they face in terms of access and affordability. The 55th Annual Conference of the Society of Nuclear Medicine India (SNMICON 2023) is scheduled November 16–19, 2023, at the Auditorium of AIIMS Jodhpur.
Global market
The global nuclear medicine equipment market is valued USD 3.28 billion in 2023, and is expected to reach USD 4.01 billion by 2028 at a CAGR of 4.14 percent.
The dominant region is North America, expected to make a significant contribution of 45 percent to its overall growth. The United States and Canada are the primary revenue-generating countries within this region. The Asia-Pacific region is projected to experience significant growth with the highest CAGR over the next five years. The key players operating in global nuclear imaging equipment market are Siemens Healthcare GmbH, General Electric Company, Koninklijke Philips N.V., Digirad Corporation, Neusoft Corporation, Canon Medical Systems Corporation, Surgiceye GmbH, DDD-Diagnostic A/S, CMR Naviscan, and Mediso Ltd.
Advances in molecular imaging technology for PET and SPECT
Six technologies are in the pipeline, and the first two were the most innovative and received the most attention in the past couple years, and potential game-changers in molecular imaging.
FAPI PET/CT. Fibroblast activation protein (FAP) is found to be overexpressed in cancer-associated fibroblasts (CAFs) in various types of tumors. With a high expression rate in more than 90 percent of epithelial tumor, FAP plays a significant role in the progression and prognosis of different cancers. Consequently, FAP is recognized as a promising target for radionuclide-based approaches in both diagnosing and treating tumors, as well as diagnosing non-malignant diseases associated with extracellular matrix remodeling.
Immuno-PET. Personalized selection of monoclonal antibodies for targeted therapy can improve clinical outcomes. Immune PET imaging enables assessment of biodistribution, tumor targeting, and prediction of efficacy and toxicity, guiding personalized treatment, and drug development. Molecular imaging using radio-labeled monoclonal antibodies allows visualization and quantification of tracer uptake, providing an imaging biomarker for target expression and tumor targeting assessment.
Movement to digital detectors and replacing photomultiplier tubes (PMT) technology. This improves image quality and sensitivity of the detector while also reducing the size and weight of scanner systems.
Expansion of the Z-axis so a patient can be imaged head-to-toe in a single scan. This allows for a reduction in radiotracer dose and exam time.
New radiopharmaceuticals being developed. These new biomarkers are developed to improve care with the prognostic value, and is integrating them into its approval process to help speed access on the market.
Movement to iterative reconstruction. Vendors in the imaging industry have shifted from filtered back projection (FBP) image reconstruction to iterative reconstruction algorithms. This transition has resulted in improved image clarity and enhanced noise reduction capabilities. The combination of these technologies has renewed interest in purchasing new nuclear imaging systems, both PET and SPECT.
AI in nuclear medicine
The role of artificial intelligence (AI) in nuclear medicine is expanding at a rapid pace, bringing about unprecedented advancements in diagnostic imaging and therapy. One notable area is in the enhancement of diagnostic imaging. Nuclear medicine relies on the detection of gamma rays emitted by radiotracers, which accumulate in specific organs or tissues, allowing physicians to visualize their function and structure. However, the generated images may sometimes exhibit low quality, posing challenges for accurate interpretation by clinicians.
To address this, AI leverages advanced algorithms and machine learning techniques to analyze the raw data obtained from nuclear medicine scans, enabling the generation of high-quality images with improved resolution and contrast. This not only facilitates more precise diagnoses but also reduces the need for additional imaging tests, thus minimizing patient’s exposure to radiation.
Another significant impact of AI is the quantification of nuclear medicine images, replacing the subjective assessment with a more objective and precise approach. Traditionally, the interpretation of these images relied heavily on the expertise and experience of physicians. However, AI extracts quantitative information from the images, enabling clinicians to obtain a deeper understanding of disease severity, monitor its progression, and assess treatment effectiveness. This objective and data-driven approach revolutionizes the field by providing more accurate and reliable measurements.
Additionally, AI is a pivotal factor in the advancement of personalized medicine within the field of nuclear medicine. By leveraging AI capabilities to analyze vast quantities of patient data, previously unnoticed patterns and trends can be identified. This has the potential to uncover novel biomarkers and facilitate the development of targeted radiotracers, enabling highly precise and individualized approaches to both diagnosis and therapy. The integration of AI in nuclear medicine thus holds immense promise in tailoring medical interventions to the specific needs of each patient.
The emerging field of theranostics, which integrates diagnostics and therapy into a single procedure, is benefiting from AI advancements. AI plays a crucial role in optimizing the selection of radiotracers and treatment planning, ensuring that patients receive personalized and highly effective therapies with minimal toxicity.
Furthermore, AI can contribute to predicting treatment response and anticipating potential side effects, empowering physicians to make well-informed decisions regarding patient care. This aspect holds significant importance, particularly in the realm of radiopharmaceutical therapy, where striking the right balance between therapeutic efficacy and minimizing toxicity is crucial.
AI has the capacity to either widen the divide in health inequity or significantly reduce it. If deployed inclusively, AI technology can help overcome geographical barriers in healthcare delivery, ensuring that general and specialized care reaches underserved communities. However, if AI technology remains limited to regions already endowed with ample healthcare access and direct availability of health infrastructure, such as radiology and nuclear medicine, it may inadvertently accentuate existing disparities.
Despite the numerous benefits of AI in nuclear medicine, several challenges within the AI pipeline require careful attention to ensure that its application remains beneficial rather than detrimental. When fully realized, AI-integrated healthcare can be integrated as an integral part of a broader strategy to converge local, national, and global efforts toward achieving health equity. The applications of AI in nuclear medicine and radiology hold the potential to emerge as powerful tools in advancing social and health equity.
Outlook
The field of nuclear medicine has witnessed significant advancements and has become a pioneering approach in medical diagnostics and treatments. The integration of AI has further revolutionized the field, enhancing diagnostic imaging, enabling objective quantification, and facilitating personalized medicine. AI-driven advancements in nuclear medicine hold immense promise for improving patient care, optimizing therapy selection, and predicting treatment outcomes. However, challenges and considerations related to equitable access, regulatory procedures, and cost-effectiveness must be addressed to ensure the beneficial and inclusive deployment of AI technology. Overall, nuclear medicine, coupled with AI, is poised to continue transforming the medical landscape, leading to improved patient outcomes and contributing to the advancement of healthcare.
Second Opinion:-
Evolution of theranostics – Going beyond radioiodine therapy.












