Daily News
Government, the savior of MRI market
With a miniscule increase in private buying, it is the government hospitals which did the major buying in 2019, and kept the Indian industry afloat.
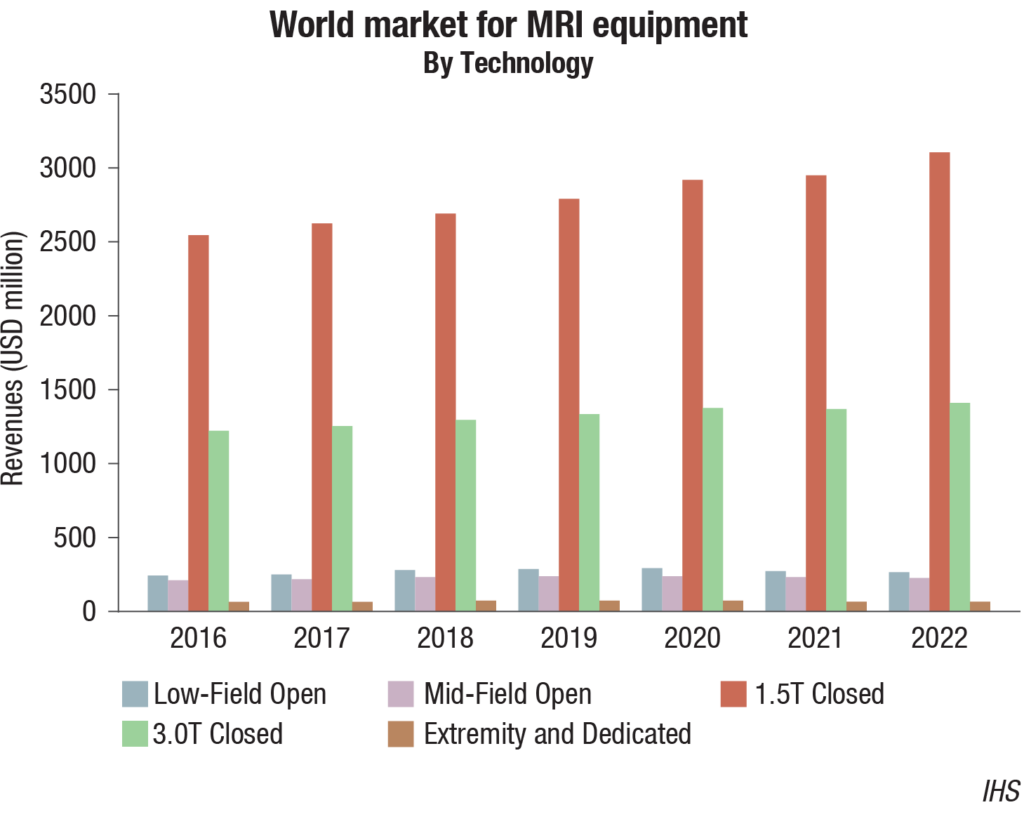
MRI systems are becoming more powerful with the quality of images improving; the patient’s comfort is now taken largely into consideration. Although the technology has improved, and purchases are now being made for the 3.0T product segment, 1.5T remains the fastest growing segment within the global MRI equipment market from 2019 through to 2022.
The purchase of MRI systems to replace existing installs may be limited in the future by the ability of healthcare providers to simply upgrade the existing install, either replacing key components or advancing software. With healthcare spending remaining under scrutiny in a number of mature and emerging markets, this could provide a cost-effective option to improve the quality of care provided, whilst limiting the financial impact of the upgrade. This may limit the growth of the future installed base, the number of units shipped, and could lead to a further lengthening of replacement cycles of MRI systems.
Indian market
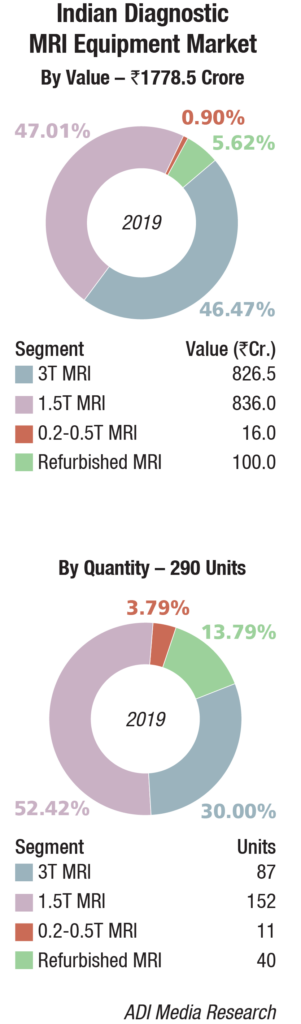 The Indian MRI equipment market for 2019 is estimated at Rs 1778.5 crore, and 290 units, by volume. It continues to be dominated by Siemens, GE, and Philips. Toshiba and Hitachi are the other aggressive brands. This estimate includes 12 percent GST and third-party items, which amount to approximately 8 percent of the price of the equipment.
The Indian MRI equipment market for 2019 is estimated at Rs 1778.5 crore, and 290 units, by volume. It continues to be dominated by Siemens, GE, and Philips. Toshiba and Hitachi are the other aggressive brands. This estimate includes 12 percent GST and third-party items, which amount to approximately 8 percent of the price of the equipment.
The premium systems 3T and 1.5T continue to dominate the market with an approximate 93 percent share by value. The 1.5T segment has the largest market share, at 47 percent by value and 52 percent share by volume, albeit the growth is coming from the 3T segment. The 0.2T-0.5T and refurbished machines and the refurbished ones are stagnant by volume, although there is a drastic drop in price realization.
In June 2018, Tata Trusts had launched a portable India-made MRI scanner, which was developed by VoxelGrids. However, this MRI machine has not gained much popularity.
Procurement from the private sector was disappointing, it is the government hospitals which did the major buying and a back-of-the-envelope calculation shows a 22 percent increase over 2018. The government hospitals are introducing measures to make the process of imaging faster and available at an affordable rate. The imperatives to shorten MRI examination without lowering image quality have become urgent. For instance, wait time of an MRI scan at AIIMS, Bhopal is for around 3 months. The hospital is ensuring that this would be reduced by more than half. In response, inventing cutting-edge technology with the focus to provide a better environment to patients is the effort of all vendors.
Major Vendors* in Indian MRI Equipment Market – 2019 |
||
| Tier I | Tier II | Others |
| Siemens, GE, and Philips | Toshiba and Hitachi | Esaote |
| *Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian MRI equipment market. | ||
| ADI Media Research | ||
Having said this, the financial viability of this segment is a big question mark, and there is an underlying perception that the segment may just be heading toward refurbished systems, which have been almost weeded out with so much effort.
Global market
The global MRI equipment market size was valued at USD 4 billion in 2019. It is anticipated to expand at a CAGR of 5.3 percent during 2020–2026, estimates Grand View Research. The rising geriatric population, number of chronic diseases, and demand for minimally invasive or non-invasive diagnostic procedures are some of the primary drivers for the MRI equipment market.
In addition, advancement in scanning techniques, such as open MRI systems, software upgrades, and superconducting magnets, are fueling the growth. Also, development of MRI systems compatible with cardiac pacemakers is propelling the demand for these instruments. With advancements in contrast agents, for instance, the paramagnetic contrast agent, gadolinium-DTPA, is used as intravenous injection to give sharp, accurate, and precise images within 20 minutes to one-hour duration.
Advancements in medical imaging devices have enhanced the diagnosis and treatment of cardiovascular diseases and cancer among other health conditions. Rising demand for minimally invasive treatment is leading to innovation in diagnostic imaging devices. Four advancements, such as accelerating processing speed, expanding the parameters of 3D and 4D, capturing images at the right place and at the right time, and automating workflow, are expected to increase the adoption of medical imaging over the next six years.
Significant increase in the number of public and private hospitals across countries, such as India and China, is boosting the demand for diagnostic imaging devices. Rising medial tourism, coupled with government initiatives in this region, is expected to boost the growth of the MRI market.
On the other hand, high cost associated with MRI systems, maintenance, and servicing is challenging the growth. In addition, stringent regulatory framework, resulting in delayed product approvals and frequent product recalls, is augmenting the degree of challenges.
The hospitals segment currently captures the largest market share and is expected to continue leading during 2020–2026, by end users. However, owing to complex infrastructural requirements of high-field MRI machines, their adoption is expected to be limited only to a number of establishments. The ambulatory surgical centers segment is expected to expand at the fastest CAGR with government initiatives to improve and increase the number of primary care centers. Mobile MRI machines provide convenience to immobile patients as well as patients in remote regions.
Rapid growth is projected in emerging markets in countries within the Middle East and Africa. The Chinese market is estimated to have been the second largest market globally in 2019 with its large population size and growing middle class, with regards to healthcare needs. Along with players becoming more prominent in the Chinese MRI equipment market, the Chinese aging population is resulting in more demand for diagnosis, using imaging products including MRI.
Major players competing in the global MRI market include, but are not limited to, Siemens, Philips, GE Healthcare, and Hitachi Medical Systems. These companies hold a remarkable position mainly due to their strong geographic reach. Some other players operating in the market include Toshiba Corporation, Aurora Imaging Technologies, Esaote, and Sanrad Medical Systems.
Market trends
MRI is the fastest growing and most versatile of all the imaging modalities. However, reducing healthcare budgets is a continuing trend, and this can sometimes deter investment toward the installation of additional MRI imaging facilities at clinical settings. Radiologists are under increased pressure to provide high-quality levels of service to patients, despite the increase in patient throughput, and the reduction of investment in healthcare provisions.
As healthcare providers become increasingly more conscientious of their budgets, more cost-effective solutions are in demand. IHS Markit projects the 1.5T product segment to be the fastest growing, with a unit compound annual growth rate of 5.1 percent. The 1.5T segment is the most popular and practical option to install within a mobile MRI trailer. The emergence of mobile MRI technology is largely driven by social, economic, and technological factors. The units consist of the trailer, which contains the MRI system, along with all technology necessary to perform the procedures, such as workstations, monitors, magnetic shielding, and climate control (air-conditioning, heating, and humidification manipulation).
Mobile MRIs
Mobile MRI units are easily transported and shared between healthcare provisions and can decrease and distribute the cost of ownership. However, renting a mobile MRI system is often seen as a temporary measure. With increase in the diagnosis of non-communicable diseases, mobile MRI can be a necessary supplement, to ensure patients are scanned and diagnosed with sufficient time to be treated competently. Mobile MRI also has the benefit of reducing costs to the patient. Investigations and research by the Canadian Coordinating Office for Health Technology Assessment (CCOHTA) has found that using mobile MRI systems can reduce the costs to the customer by more than 50 percent. Calculated and estimated costs include average travelling expenses, and the patient’s and staff time spent per scan.
The flexibility and transportable nature of a mobile MRI unit enables access to patients who might not normally be able to receive an MRI scan, such as those of rural locality, and those patients who are less mobile.
Mobile imaging solutions offer flexibility, (location) and risk mitigation, (no installation outlay) to organizations looking to improve their care delivery and to support expansion facilities. However, mobile MRI may not be the correct option for all organizations. There have been several modifications made to MRI that have made it more conducive to mobile technology. Over the past several years, the units have become lighter, smaller, self-shielding, and it is now possible to mobilize superconductive 0.5T or 1.0T MRI units. Originally, the preparation time necessary to set up mobile MRI units was lengthy, which impacted scheduling. Newer MRI units require minimal set-up and the magnet, which often needed to be ramped after each move, is now ramped during the initial calibration and remains ramped throughout each move.
Purchasing decisions of mobile technology should not only be based on costs, but the opportunity to provide MRI services to clinical settings in close proximity, that alone could not fully utilize the technology. Future population and health trends also need to be factored into the decision. The aging population of the world is increasing with life expectancy to be around 69 years.
The total cost of a mobile MRI is in some cases still lower than that of a fixed site. The average selling price of the total MRI equipment market will decline by a CAGR of –2.7 percent from 2019 to 2022. This decrease will be reflected in the total cost of a mobile MRI system, which can already be a more cost-effective solution than a fixed MRI system. Although there are increased operating costs with mobile MRI technology, these costs can be offset by increased throughput and flexibility.
Mobile MRI is increasingly becoming a viable option for clinical settings in rural locations, with shared ownership of the machines between various organizations. However, due to the costs of the maintenance and upkeep of the mobile units, in addition to the expenses associated with the transportation of the trailers, the uptake of the machines in emerging and less economically stable markets, financially, may not yet be an option.
Research update
Deep-learning, a type of artificial intelligence, can boost the power of MRI in predicting attention-deficit hyperactivity disorder (ADHD), according to a study published in Radiology: Artificial Intelligence. Researchers said the approach could also have applications for other neurological conditions. The human brain is a complex set of networks. Advances in functional MRI, a type of imaging that measures brain activity by detecting changes in blood flow, have helped with the mapping of connections within and between brain networks. This comprehensive brain map is referred to as the connectome.
Brain MRI has a potential role in diagnosis, as research suggests that ADHD results from some type of breakdown or disruption in the connectome. The connectome is constructed from spatial regions across the MR image, known as parcellations. Brain parcellations can be defined based on anatomical criteria, functional criteria, or both. The brain can be studied at different scales based on different brain parcellations.
Prior studies have focused on the so-called single-scale approach, where the connectome is constructed based on only one parcellation. For the new study, researchers from the University of Cincinnati College of Medicine and Cincinnati Children’s Hospital Medical Center took a more comprehensive view. They developed a multi-scale method, which used multiple connectome maps based on multiple parcellations.
To build the deep-learning model, the researchers used data from the NeuroBureau ADHD-200 dataset. The model used the multi-scale brain connectome data from the project’s 973 participants along with relevant personal characteristics, such as gender and IQ. The multi-scale approach improved ADHD detection performance significantly over the use of a single-scale method.
By improving diagnostic accuracy, deep-learning-aided MRI-based diagnosis could be critical in implementing early interventions for ADHD patients. The approach also has potential beyond ADHD.
In the future, the researchers expect to see the deep-learning model improve as it is exposed to larger neuroimaging datasets. They also hope to better understand the specific breakdowns or disruptions in the connectome, identified by the model that are associated with ADHD.
New MRI technique predicts dementia in stroke patients. A new MRI technique using diffusion tensor imaging (DTI) can help predict when patients might suffer from stroke-related dementia, according to new research published in Stroke: A Journal of Cerebral Circulation. The authors found that a single MRI scan could provide key information about damage to a patient’s brain. Comparing those findings to a healthy patient’s imaging results helped the team differentiate healthy and damaged tissue. The study included 99 patients with small vessel disease caused by ischemic stroke. The average patient age was 68 years old. All patients were enrolled in the St. George’s Cognition and Neuroimaging in Stroke (SCANS) study from 2007 to 2015, which involved receiving MRI scans for three consecutive years and “thinking tests” for five consecutive years. Overall, study participants showing signs of the most brain damage was more likely to develop problems with their thinking. Eighteen participants developed dementia during the study, and the average time to onset was approximately three years and four months.
The study did have certain limitations, according to the statement. The healthy patient MRI scans used for comparisons all came from the same patient, for example, and all study participants had small vessel disease that came from suffering the same kind of stroke, so the results may not apply to people with different forms of the disease.
Is MRI better than angiography for diagnosing, treating certain heart attacks? Cardiac MRI may better assess and treat patients who have experienced a type of heart attack caused by an extremely narrowed artery compared to standard angiography, reported authors of a May study published in Circulation. Overall, the use of MRI led to a new diagnosis involving a damaged artery in 30 percent of patients, and a diagnosis unrelated to the artery in another 15 percent, reported John Heitner, MD, director of noninvasive imaging at NewYork-Presbyterian Brooklyn Methodist Hospital, and colleagues. Heitner et al. explained that it can be hard for physicians to identify the damaged artery responsible for a non-ST segment elevation myocardial infarction (NSTEMI). Typically their first choice is coronary angiography, with MRI only considered afterward and if results remain unclear. We suspected the MRI’s ability to directly visualize the heart muscle that was affected could improve accuracy, and our research suggests that to be the case. One-hundred and fourteen patients were enrolled in the study, all had presented with their first heart attack at one of three centers. Everyone underwent an MRI and subsequent angiography; images were independently and blindly reviewed to locate the clogged artery responsible for the heart attack. Readers could not identify the blocked artery using angiography in 37 percent of patients. Of that group, MRI successfully located the artery in 60 percent of patients, or led to a new non-coronary artery disease diagnosis in 19 percent. Among cases when angiography successfully found the blocked artery, MRI found a second artery in 14 percent and a non-CAD diagnosis in another 13 percent. “This study suggests that using an MRI should be the standard practice in NSTEMI patient diagnosis and care,” Heitner said. “We want to make sure that we are treating the artery that caused the heart attack as this will likely lead to better long term outcomes for the patient.”
Technology update
A new 3D MRI computing technique developed by scientists in WMG at the University of Warwick focuses on hierarchical template matching (HTM) to diagnose cardiac disease without the use of gadolinium contrast. The technique is explored in an article in the journal Scientific Reports. Traditionally, when a patient goes for an MRI scan, they are given a dose of gadolinium, which reacts with the magnetic field of the scanner to produce an image of the protons in the metal realigning with the field. The faster the protons realign, the brighter the image features to show where the dead muscles are in the heart and what the diagnosis is. The dose of gadolinium, however, can have detrimental effect on other parts of the body, particularly the risk of kidney failure.
The hierarchical template-matching technique involves a numerically stable technique of left ventricular (LV) myocardial tracking; A 3D extension of local weighted mean function to transform MRI pixels; and a 3D extension of the HTM model for myocardial tracking problems. Use of this technique eliminates the need for gadolinium, reducing the risk of damage to other organs.
“Using 3D MRI computing technique, we can see in more depth what is happening to the heart, more precisely to each heart muscle, and diagnose any issues, such as remodeling of the heart that causes heart failure. The new method avoids the risk of damaging the kidney opposite to what traditional methods do by using gadolinium,” says Prof. Mark Williams from WMG at the University of Warwick.
“This new MRI technique also takes away stress from the patient, as during an MRI the patient must be very still in a very enclosed environment, meaning some people suffer from claustrophobia and have to stop the scan. Often when they do this, they have to administer another dose of the damaging gadolinium and start again. This technique does not require a dosage of anything, as it tracks the heart naturally,” added Jayendra Bhalodiya, who conducted the research from WMG, University of Warwick.
Way forward
Works in progress run the gamut from whole MRI systems to components designed to improve workflow. Some promise to bring data to mobile devices, such as cell phones and tablets. The question is whether these new ideas will turn into real products or if they are just hopeful embellishments of where technology might go. A lot is at stake.
The manufacturers of MRI equipment have to anticipate where markets are going, just as quarterbacks have to throw to where a receiver is going, not to where he has been. But they have to be careful. Neither can be taken in by head fakes.
For-profit companies eventually have to make a profit. And making the world a better place is not their top criterion. That is not to say profitable businesses do not make the world better. They did so when it came to MRI and other high-tech – as well as low-tech – imaging modalities.
But imaging undeniably has made healthcare more expensive. Yes, heroic measures like exploratory surgery are seldom, if ever, done anymore. But that kind of surgery was never commonplace. And for good reason.
Not only were exploratory surgeries difficult for patients to bear physically, they added expense, gobbling up operating room and staff time, and incurring costs as patients were hospital-ridden for days or weeks. MRI, on the other hand, has been widely used for decades.
As often happens with any new technology, MRI reimbursements were high in those early days. Not surprisingly, the number of MRI scanners installed spiked in the following decades. But the number began to ebb as the market grew saturated and reimbursements declined. Still MRI remains popular.
Even though medical practice around the globe is changing, such that value – not reimbursement – is becoming the most important factor. But cost will remain an issue, because it will factor into the calculation of value.
And so, MRI has come to a fork in the road. It stands either on the cusp of renewed greatness or on the periphery of a bubble ready to burst. Or it could just stand there – paralyzed – at that fork.
Time – and the development of MR technology – will tell.












