Ventilators
Ventilators Continue With Their Path Of Evolution
As patients’ needs change, so does the optimal ventilation strategy.
Ventilators have evolved significantly to optimize improvement in gas exchange while minimizing ventilator-associated lung injury. With technological advancements, the terminology has become more complex, contributing to possible confusion for the clinician. Modern mechanical ventilation allows the manipulation of every aspect of inspiration while expiration is not altered except for the magnitude of positive end-expiratory pressure applied.
Given the lack of significant evidence regarding the superiority of one mode of mechanical ventilation over another in improving clinical outcomes, including mortality, the selection of the initial mode is usually based on clinical familiarity, institutional preference, and available technology.
Indian market dynamics
The Indian ventilators market in 2018 is estimated at 9250 units, valued at ₹487 crore. The imported equipment continues to dominate the segment with a 79 percent share by value, and a 63.8 percent share by units. The imported segment saw an 18 percent increase over 2017 and the indigenous segment by about 15 percent. The transport and ambulatory segment, in spite of the directive that every ambulance must be equipped with a ventilator, saw a marginal increase in 2018. The refurbished segment defies global trends, and continues to have relevance in the Indian market. The vendors maintain that as long as they are able to guarantee availability of spare parts, service within 24 hours, and maintain goodwill with their customers, including large hospitals, this segment shall thrive. The popular brands are Maquet, Draeger, GE, Carefusion, and Belavista, the latter two now under the Vyaire umbrella. The compressor models are more popular as the reliability of a turbine-based refurbished model is in question.
Maquet continues to dominate the segment with its top-of-the-line models. Draeger is a close second, having had major success with its Savina series in the bids invited by the government hospitals in 2018, one of the large orders being 150 units by state of Gujarat. It continues to do well in 2019.
| Tier I | Tier II | Tier III |
|---|---|---|
| Maquet and Draeger | GE, Schiler, and Hamilton | Mindray, Carefusion Covidien Philips, Air Liquide, and Skanray |
| *Vendors are placed in different tiers on the basis of their sales contribution to the overall revenues of the Indian Ventilator market. | ||
| ADI Media Research | ||
GE, Schiller, and Hamilton remain aggressive with a market share in the vicinity of 5 percent each, by value. Hamilton seems to have been shortlisted for a tender invited by the government for 1186 units; orders are expected to be placed in 2019. Mindray has a pan-India presence and is making steady progress. Its exclusive tie up with Narayana Hridyulaya for about 65 systems annually is encouraging. Vyiare, having completed its merger with Carefusion and Acutronic, is expected to have an aggressive presence in 2019.
Technology trends
The computer-based technology has made the modern-day ventilators more doctor and patient-friendly. The synchronized ventilators, with volume control and volume guarantee with advanced pulmonary graphics, have helped to wean away from ventilators easier with lesser side effects. Now ventilators can be connected with central monitors and monitored from a distance as well. The concept of E-ICU wherein the monitoring system is electronic, digital, and real time is likely to pick up in the near future.
On the other hand, the concept of gentler ventilation has increased the demand of a CPAP system and heated humidified high-flow nasal cannula (HFNC). Many neonatal and pediatric conditions are helped by these relatively simple ventilation techniques. There is more scope for high-frequency ventilators in current-day NICU and PICU care, and the need is to have cost-effective, high-frequency ventilators. T-piece resuscitators have replaced self-inflating bags in labor rooms and they are being used as transport ventilators also. With the rising cost of intensive care and many sick children requiring home ventilators, there is a dire need to build an appropriate medical support system to help such practices.
From the latest scenario, it has been noted that the intensivists are rapidly moving toward non-invasive ventilation (NIV) and high-flow oxygen therapy (HFOT). The addition of HFOT to ventilator makes this technique more widely available and implementable with no extra cost to it. In recent times, HFOT has migrated into the home care environment owing to the availability of portable HFNC standalone devices in the market. However, in a hospital environment, it is being preferred as a feature or a mode for smooth transition of NIV to invasive ventilation, as and when required, in high-end mechanical ventilators. HFNC is also proving helpful in supporting the oxygenation of hypoxemic patients and is being well-tolerated by children. Today, most of the mechanical ventilators are equipped with HFNC/oxygen therapy. HFNC expands the ventilator’s capacity during the pre- and post-intubation stages. A positive clinical effect on various respiratory parameters has been observed after the usage of HFNC and studies suggest that it may reduce the work of breathing as well.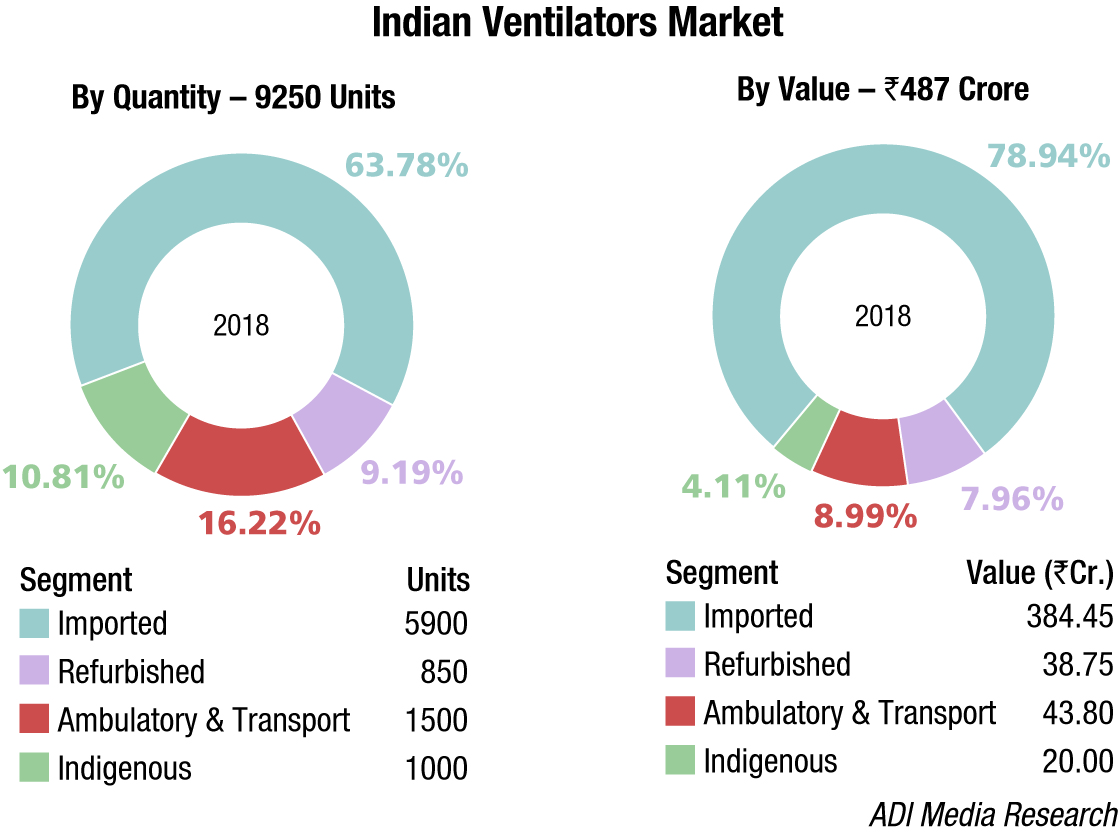
Patient-ventilator asynchrony exists when the phases of breath delivered by the ventilator do not match those of the patient. Current evidence suggests that the best approach to managing asynchronies is by adjusting ventilator settings. Proportional modes improve patient-ventilator coupling, resulting in greater comfort and less dyspnea, but not in improved outcomes with respect to the duration of mechanical ventilation, delirium, or cognitive impairment. Advanced computational technologies will allow smart alerts, and models based on time series of asynchronies will be able to predict and prevent asynchronies, making it possible to tailor mechanical ventilation to meet each patient’s needs throughout the course of mechanical ventilation.
Patients’ needs are changing with time because of the evolution of both pathology severity and treatments. Therefore, an optimal ventilation strategy is an adaptive process, aiming to treat the acute condition and support the gradual weaning from the ventilator or adjust to the natural fluctuations of chronic disorders. To reach the goals, advancement of bioengineers’ understanding in pathophysiology, medicine, and engineering must be combined with an interdisciplinary approach to fully address the complexity of mechanical ventilation for further improving patients’ treatment.
| Segment | Brand |
|---|---|
| Imported | Maquet, Draeger, GE Healthcare, Schiller, Philips, Mindray, Skanray, Covidien, Hamilton, Air Liquide, Vyaire, Nidek, and ResMed, Fabian HFO, Oricare (Rohanika), BPL, Aeon Med, China; Meditek, UK; and IMT Medical |
| Indigenous | Skanray, Max Meditech, Medisys (Premier), and Air Liquide |
| Refurbished | Zigma, SOMA, Technomed, and Unitech; Vision Healthcare, Ahmedabad; and SV Medisystems, Haryana |
Way forward
Modes of mechanical ventilation have shown a steady evolution over the last four decades. They have increased in complexity as engineers attempt to add technical capabilities that better serve clinical goals. The modes are combinations of volume-controlled, pressure-controlled and pressure-support breaths, mandatory/assisted breaths, and invasive and non-invasive supports.
Currently, the work on lung-protective tools and open-lung ventilation strategy to prevent alveolar collapse and maintain optimal recruitment are gaining high importance. Manufacturers are coming out with proprietary modes that target on work of breathing and amplify the patient’s ventilatory effort, thus giving freedom to adopt his own breathing pattern, which helps in quicker weaning from the ventilator. Ventilator graphics constitute a valuable tool and provide thorough understanding of the associated problems, patterns, and possible corrections to provide high-quality care.
Future ventilators will have smart algorithms that will project the trend and estimated weaning time, based on patient history. More intelligence will be built into the alarm-management system, which not only ensures safety but is also capable of warning about potential hazard. Remote monitoring of critical parameters will help ease the work of doctors as well as service personnel. Technological advancements will reduce the footprint of ventilators while enhancing the features with advanced blowers and smart batteries that can really work for long hours, independent of pneumatic and electrical source.
The product segment is not yet done with its journey of evolution!
Second Opinion
Modern-day ventilation: Artificial to personalized
Dr Niraj Tyagi
Consultant – Critical Care
SGRH
Mechanical ventilation is the corner stone of management in patients with acute respiratory failure. As our understanding about disease processes, particularly ARDS, is ever evolving so is the recognition of new dimensions of ventilator-associated lung injuries. CESAR trial done during 2009 H1N1 Influenza pandemic highlighted the importance of using protocol-driven lung-protective ventilation strategies in order to achieve improved patient outcomes. The dogma of invasive ventilation for all kinds and severity of respiratory failure has definitely faded away and today most of us are happily inclined to use noninvasive ventilation with increasing frequency. Noninvasive ventilation is one of those rare medical technologies that both improves patient outcomes and reduces treatment costs, if chosen at right time and on right patients.
The biggest challenge that our country faces in terms of managing such severely ill patients, who require highest level of monitoring and care, is the availability of adequately trained nurses and other allied healthcare associates. Most hospitals in India still do not have respiratory therapists who in the Western world share relatively major burden of implementing ventilatory strategy, and as such intensive care clinicians get very limited support when it comes to this aspect of patient care. Despite all the attempts to minimize duration on mechanical ventilation, it is still agreed that 40 percent of the total duration of mechanical ventilation is taken in weaning process.
The answer to these complex challenges is choosing wisely from all the available technology as per requirements of the institute and the unit, depending on intended usage and kind of patient population it caters to. While it can be overwhelming trying to keep up with all the so-called new modes of ventilators being coined with increasing frequency, one must recognize that the idea today is to provide an individualized ventilatory support that adapts to changing lung mechanics. This is made possible by closed-loop integration of measuring lung properties like resistance and elastance while delivering mechanical breath and making right adjustments with respect to changes in either of them.
Present-day ventilators allow flexibility of giving both noninvasive and invasive ventilation with the same machine, and the user interface allows the clinician to have a real-time assessment of lung condition.












